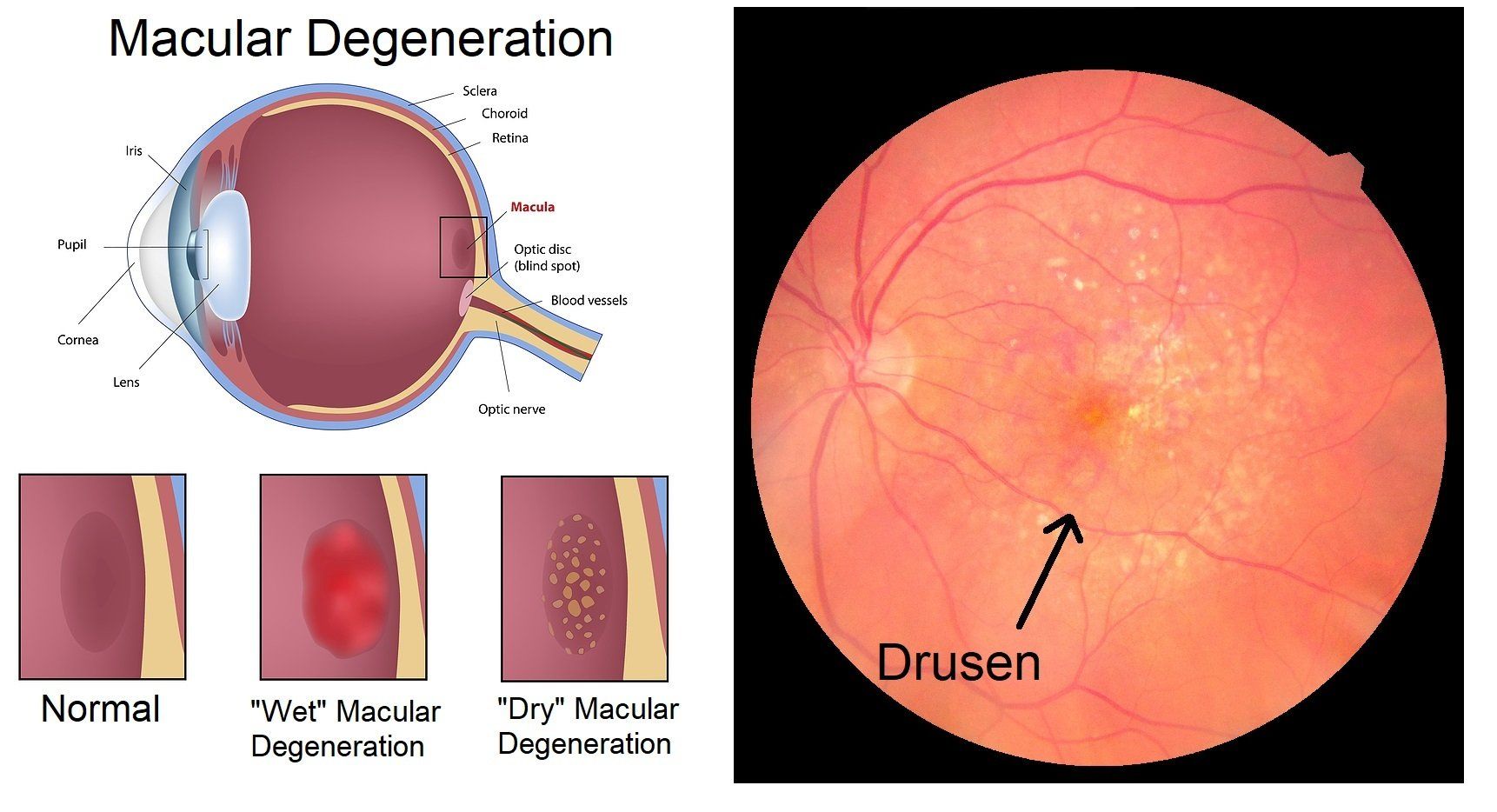
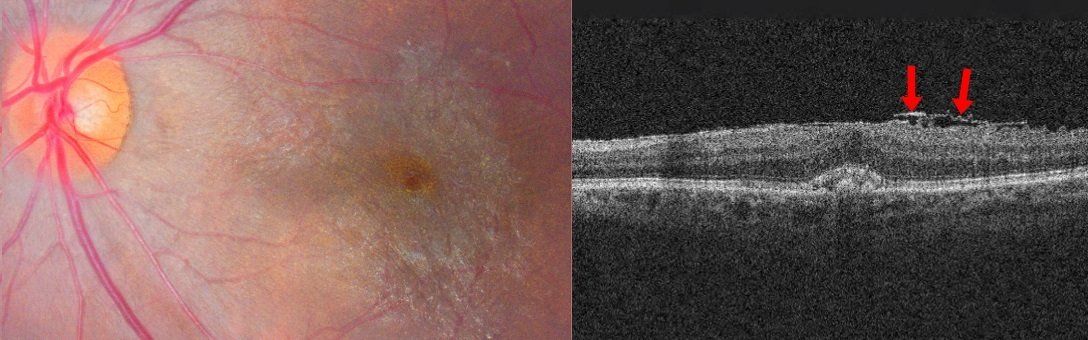
Age-Related Macular Degeneration (ARMD) is an eye disorder where there is a physical and functional deterioration of the photoreceptors (cones and rods) in the macula that is usually associated with age.
Amblyopia
Amblyopia or a “lazy eye” is where a weak eye sees poorly compared to the other eye because of a poor neurological connection to the weaker eye when both eyes have the proper eyeglass prescription. The poor vision is also not related to any eye disease. It is caused by visual deprivation to an eye during early neurological development between the eye and visual cortex of the brain. During infancy and early childhood development the visual cortex is forming neurological connections to the eyes. If an eye is deprived of visual stimuli at this time, a strong neurological connection is not formed or “hard-wired”. In other words, the brain will permanently “tune out” a bad eye because it never got“clear reception” from it. Treatment involves removing the source of visual deprivation and patching of the stronger eye. This treatment is much more successful when done at an early age. Amblyopia occurs in 2 out of every 100 children. This is why it is strongly recommended that every child get an eye exam sometime between the ages of 3 to 5 years old.

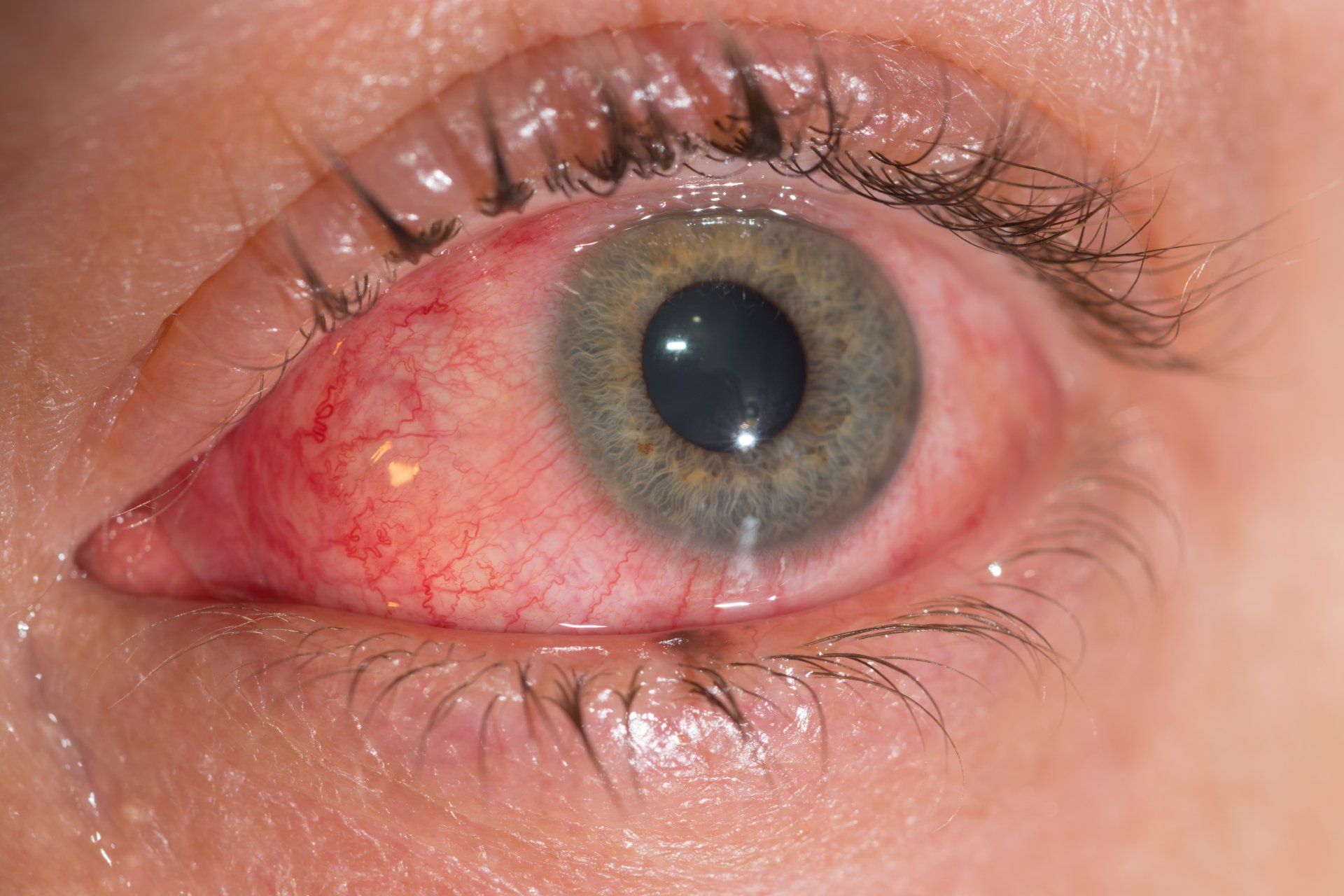
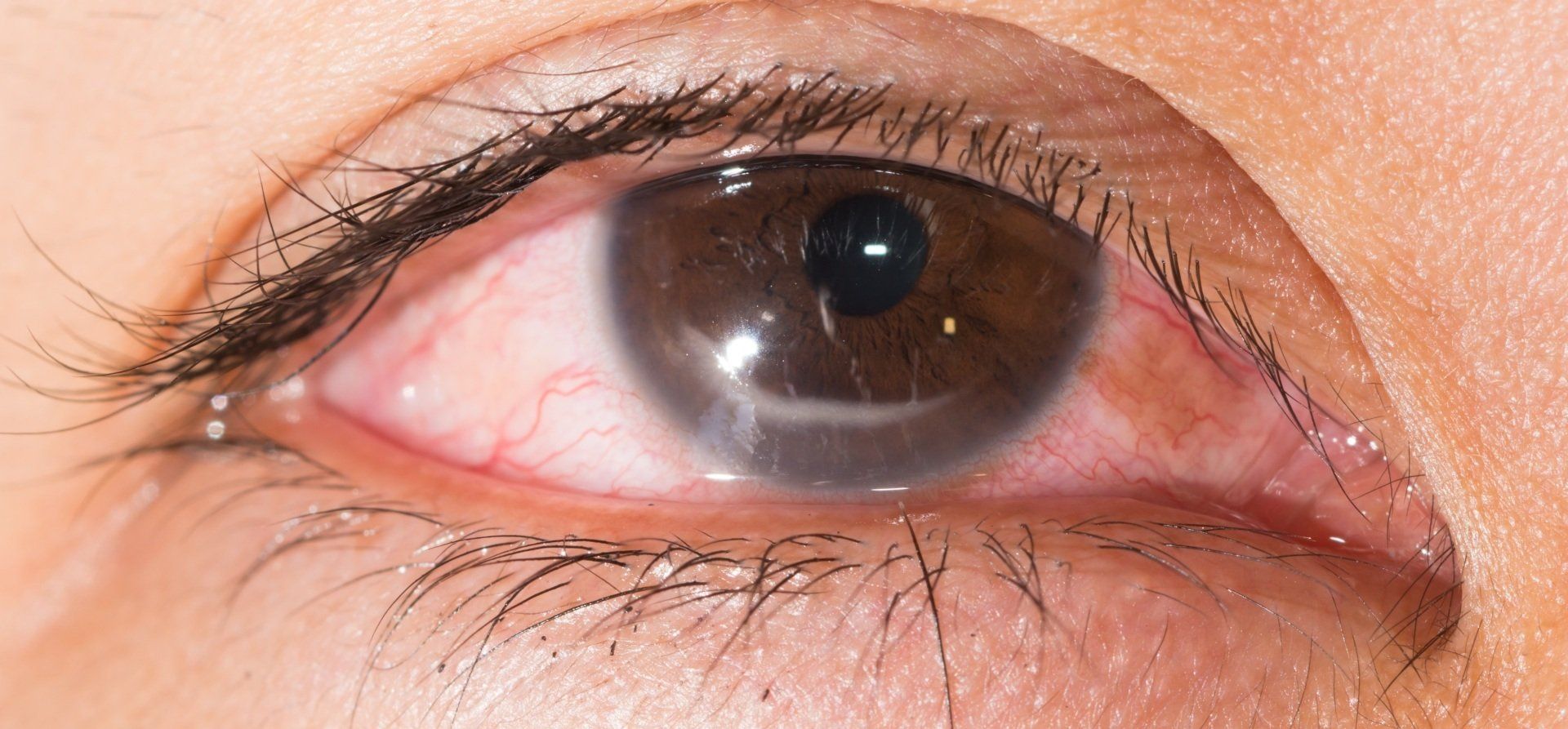
Anterior Uveitis
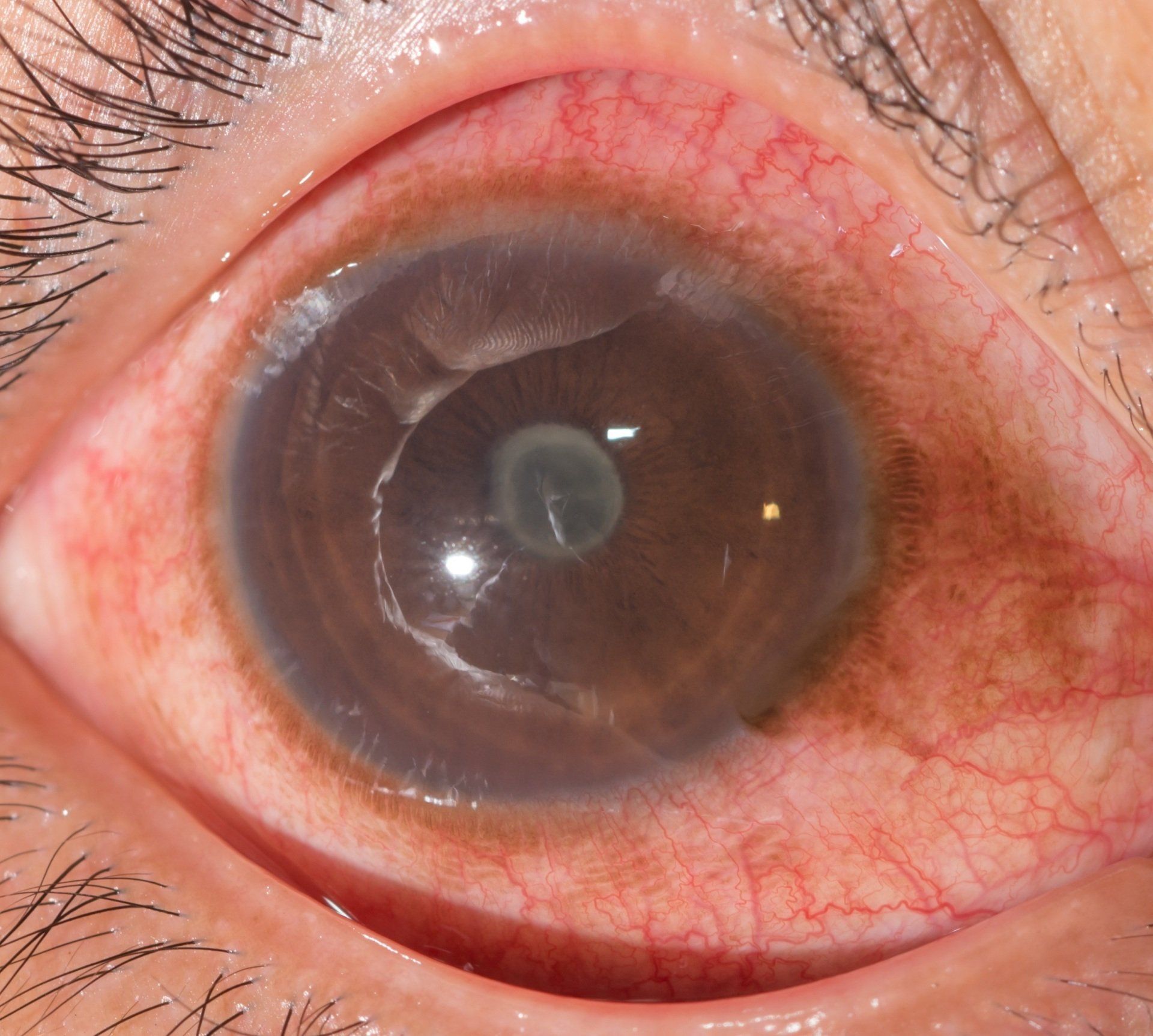
Anterior uveitis is inflammation of the uvea. The anterior or front structures of the uvea include the iris and ciliary body. Symptoms include a red and inflamed eye, light sensitivity, floaters, blurry vision and an irregular shaped pupil. It is often caused by autoimmune diseases, infections and ocular trauma. Steroids are often used to treat anterior uveitis, however, they should be used judiciously when an infection related cause is suspected.
Blepharitis
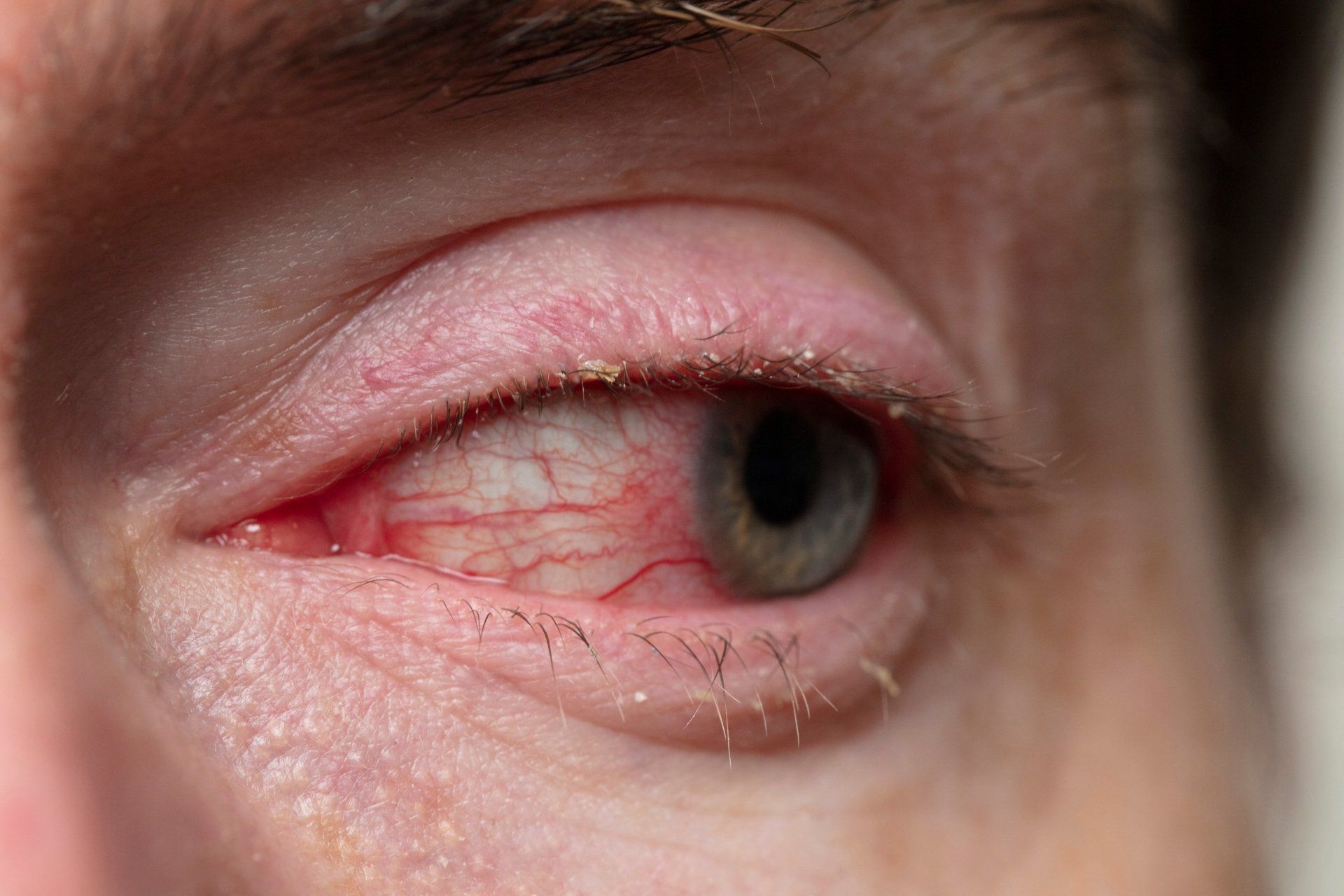
Blepharitis is inflammation of the eyelids. It is caused by bacteria on the eyelid margin and/or seborrheic dermatitis (excess oil production). The infection and excess oil production lead to inflammation, which causes irritation, dryness and redness. It is very common in the elderly and those with poor hygiene. Symptoms usually include scratchiness, itching, burning, foreign body sensation, and excess tearing. Crusty debris and flakes can be found on the eyelids around the eyelashes, especially upon waking. Sometimes the eyelids can even be stuck together upon waking. Treatment involves improving eyelid hygiene with scrubs and sometimes antibiotics.
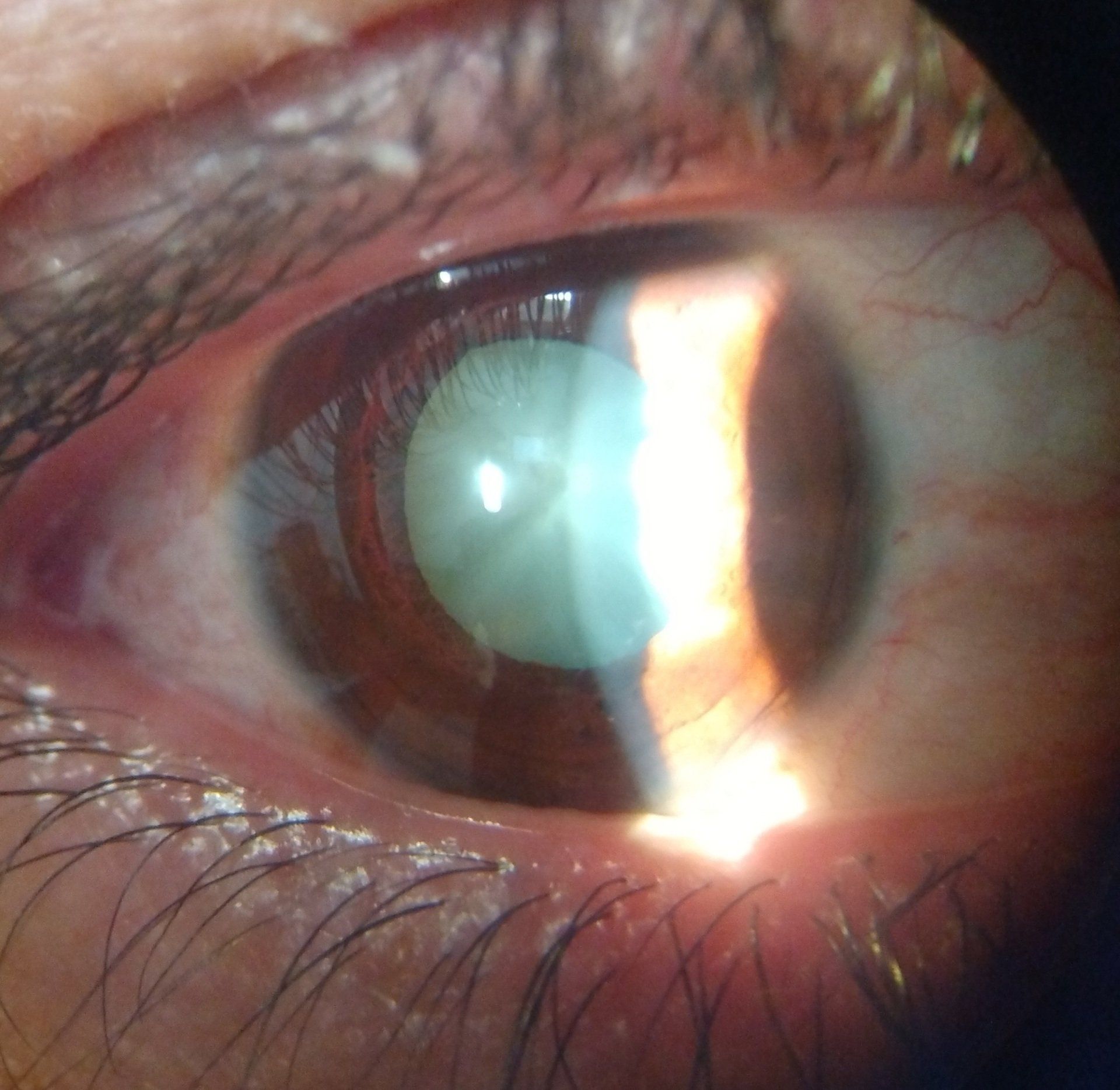
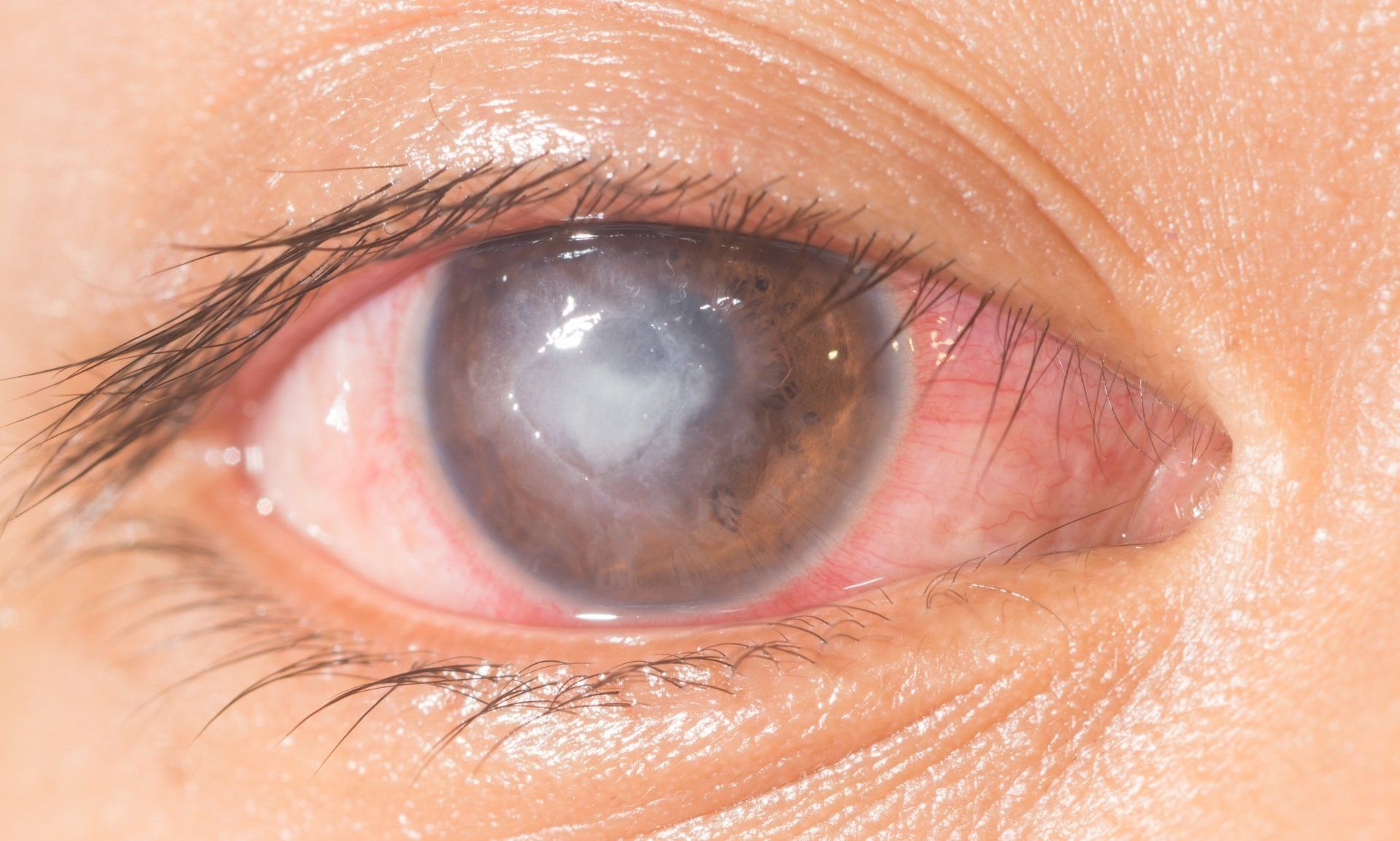
Cataracts are a clouding of the crystalline lens. The crystalline lens is located just behind the iris and helps to focus light on the retina. It is attached to the ciliary muscle by zonules. When the ciliary muscle contracts tension is released on the zonules and the crystalline lens grows in axial length. This increases the power of the eye and enables us to focus on objects at a near distance.
Chalazion
A chalazion is a red, painless lump that occurs due a blockage of an oil gland at the edge of the eyelid. A distinguishing characteristic between a stye and chalazion is that a stye is painful to the touch. Chalazions are associated with chronic blepharitis, rosacea, styes and seborrheic dermatitis. Large ones might cause watering and decreased vision from putting pressure on the eye. They also mostly happen in adults. To evaluate a chalazion your eye doctor will take a careful history and examine your eyelid with a biomicroscope. It usually takes 4-6 weeks for a chalazion to resolve on its own. To speed up resolution, warm compresses can be used 4-6 times a day to open up the gland. In persistent cases the chalazion can be injected with steroids or surgically removed.

Coloboma
A coloboma is a congenital condition of the eye where it fails to form completely. It leaves the bottom structures of the eye missing. They look as if there is a notch in the lower part of the eye and have a "keyhole" appearance. Colobomas can occur from the iris all the way back to the optic nerve head. Vision and visual fields can be significantly compromised depending on which structures of the eye are affected. Light sensitivity is also common. Nystagmus, retinal detachments, cataracts myopia and glaucoma are more prevalent. Management of a coloboma includes refractive correction, sunglasses, cosmetic contact lenses and low vision aids.


Conjunctivitis is an inflammation of the conjunctiva (the mucus membrane that covers the white colored part of the eye). It is often called "pink eye". Common signs and symptoms include redness, light sensitivity, foreign body sensation, itchiness and burning. It may be caused by numerous factors from a viral or bacterial infection, allergies, dry eye syndrome, or improper contact lens wear. Treatment ranges from artificial tears, cold compresses, removing the cause, medications and/or changing contact lens wearing habits.
Conjunctivitis.pdf
Corneal Abrasion
A corneal abrasion is a surface scratch or cut in the cornea. They are very painful, cause light sensitivity and result in excessive tearing. The vast majority of corneal abrasions are from accidental causes like getting poked in the eye or wearing a torn contact lens. The best treatment includes putting on a bandage contact lens to aid healing and decrease pain, giving an in office cycloplegic drop to relax the eye and topical antibiotics to prevent an infection.
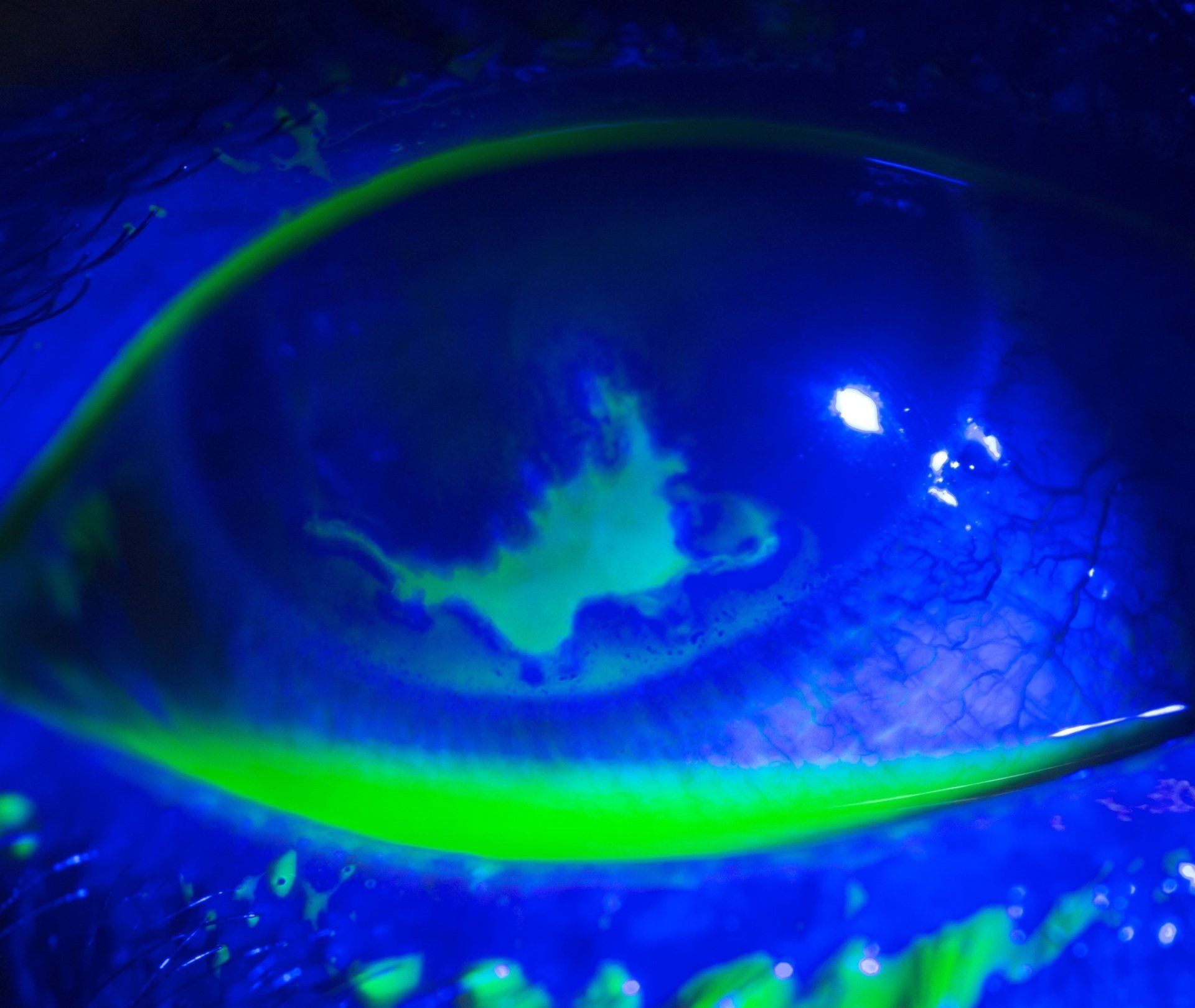
A corneal ulcer is an erosion or open sore that has penetrated the cornea’s epithelial (skin) barrier. It usually appears as a white or gray lesion in the cornea. Symptoms include pain, light sensitivity, redness and decreased vision. Causes usually involve some type of breakdown of the skin layer that protects the cornea from invasion of a pathogen. Your eye doctor will look at your cornea and eye very carefully with a biomicroscope. Treating a corneal ulcer usually starts with trying to identify the cause and then using the appropriate medication. Bacteria and viruses are the most common causes of an ulcer, but they can also be caused by fungus or parasites. Ulcers that are vision threatening, large or unresponsive to treatment should be cultured and referred to a corneal specialist promptly.
Corneal Ulcer.pdf
Dermatochalasis
Dermatochalasis is excess and loose skin on the eyelid and around the eye. It is most commonly seen in middle age and the elderly. The incidence is also higher with a history of facial injury or surgery, higher body mass index, smoking and sun exposure. Most commonly it affects the upper eyelids, but can also be seen on the lower eyelid. In most situations dermatochalasis is cosmetic, but in more dramatic presentations it can block the individual's upper peripheral visual field. A blepharoplasty by an oculoplastic surgeon is the best treatment option. In cosmetic cases it's rarely covered by insurance, however, with documentation that it blocks part of the upper visual field it may be covered.

A quality tear film is essential for good vision and for nourishment of the eye’s surface. In dry eye syndrome (DES) there is a decreased quantity or quality of the eye's natural tears that leads to a drying of the ocular surface. It is typically chronic, very common and more prevalent as we get older. Symptoms include a foreign body sensation, scratchiness, redness, watering, and burning There are numerous causes of dry eye that include systemic diseases, hormone changes, medications, LASIK and the environment. Testing for dry eyes measures the amount of tear the eye secretes and assesses the quality of the tear film. Treatment includes the use of various types of artificial tears, eye ointments/gels, punctal plugs and medicated drops.
Dry Eye Syndrome.pdf
Duane Syndrome
Patients with Duane Syndrome have a congenital disorder where their horizontal eye movements are limited or not present. It can occur in either looking in towards the nose or looking out towards the ear. It is caused by congenital problems with muscles or the nerves that innervate them. It can result in double vision when looking in the affected gaze. Surgery is not a good form of treatment. Prism and a spectacle prescription offer the method of treatment.
Image courtesy of: Jmarchn, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons

Ectropion
Ectropion is a condition where the eyelid turns outward or away from the eye. It leaves part of the eye and eyelid surface exposed. The exposure leads to dryness, redness, irritation, decreased vision and potential scarring. It is much more common in the elderly as the skin around the eye loses its elasticity. Ectropion is treated with lubricating drops, ophthalmic ointments and lid surgery to move the lid back to the eye.
Entropion
Entropion is a condition where the eyelid turns inward. A big problem with this is that it creates contact between the ocular surface and the lid margin. A common problem is that eyelashes rub up against the conjunctiva and cornea. This can lead to abrasions, redness, irritation, decreased vision, infections and potential scarring. It is also a condition that is more common in the elderly and because of a loss in elasticity of the skin around the eye. Lubricating drops, ophthalmic ointments and eyelash epilation can help temporarily. However, surgery is the best method to permanently treat entropion.
Epiretinal Membrane
An epiretinal membrane, also called macular pucker, is a fibrocellular membrane that forms on the top layer or surface of the retina. Most patients that have them are asymptomatic. However, when they form over the macula or our central vision they can cause decreased and distorted vision. In most cases an epiretinal membrane is evaluated regularly with a dilated eye exam and distortion is checked with an Amsler Grid. In significant cases a surgical procedure is performed that peels it off of the retina by a retinal specialist.
OCT Image courtesy of: Jmarchn, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
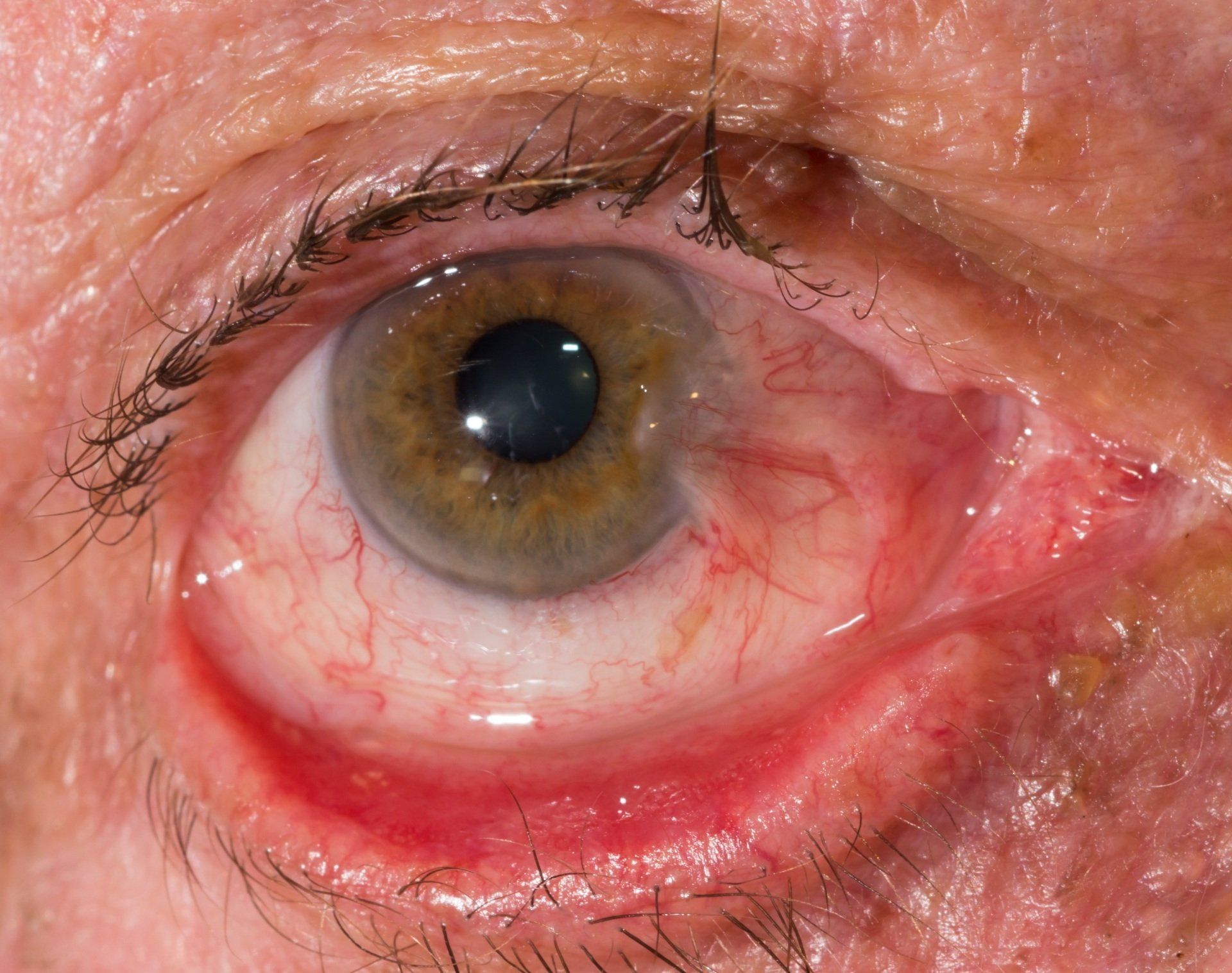
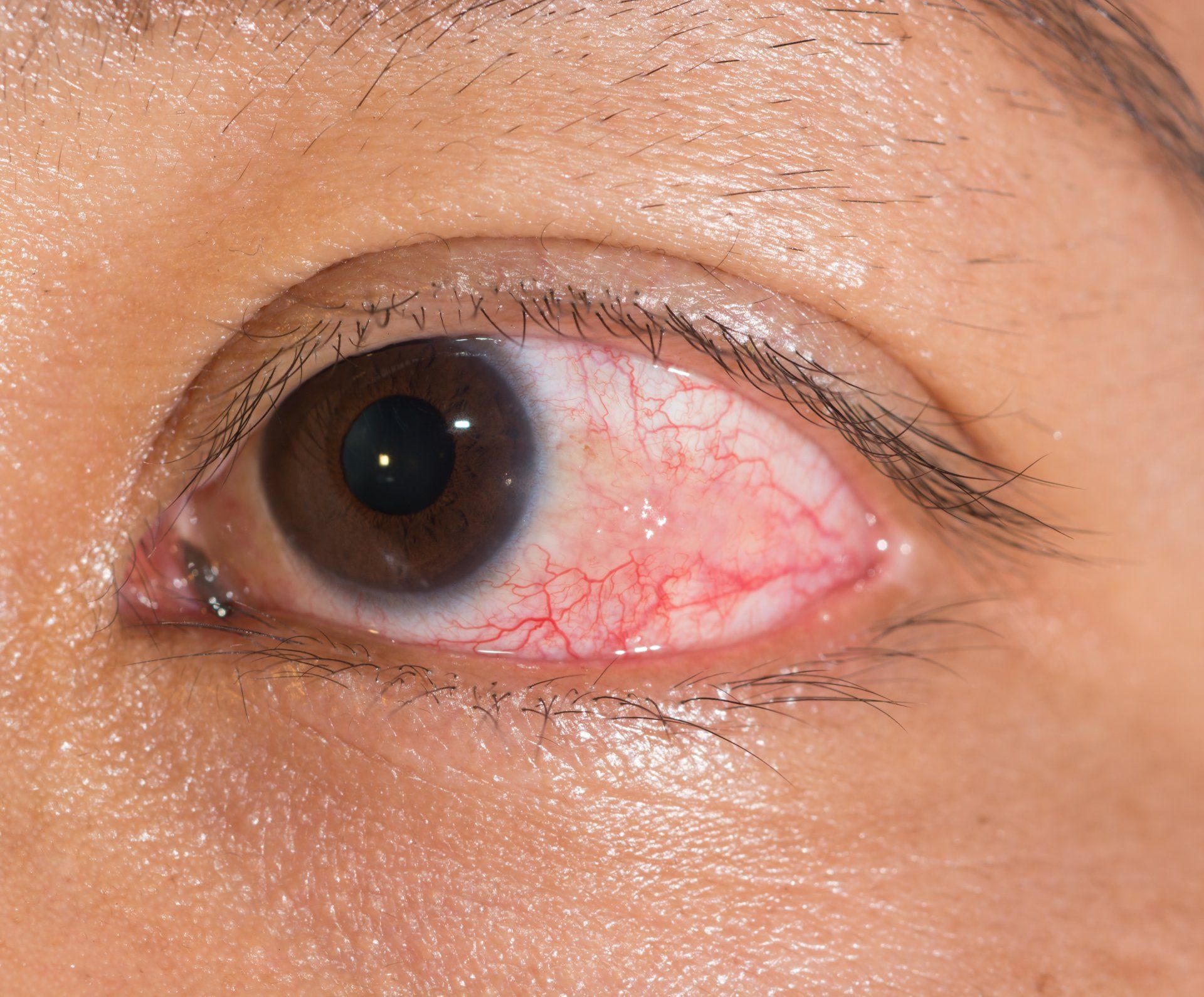
Episcleritis
Episcleritis is inflammation of the episclera. The episclera is the upper layer of the sclera. On initial appearance it looks like conjunctivitis, but the inflammation is deeper. Episcleritis occurs in a simple form that occurs in a small section of the eye or in a raised nodule. In a lot of situations it is the result of autoimmune diseases like lupus, rheumatoid arthritis, Crohn’s disease, ulcerative colitis or psoriatic arthritis. Treatment often is supportive, but mild use of topical NSAIDs and "weak" steroids can be used.
Epithelial Basement Membrane Dystrophy
Epithelial basement membrane dystrophy is also called map-dot-fingerprint dystrophy because of the unique shapes the condition shows in the cornea. It occurs because the adhesion skin cells in the cornea have to their basement membrane is poor. It mostly happens in adults. Patients may not have any symptoms. However, if the skin cells come off or erode due to their poor adhesion patients can have extreme pain, foreign body sensation, decreased vision and light sensitivity. The first time the skin cells come off it is left to heal and treated with a bandage contact lens, artificial tears and preventative antibiotics. However, recurrent erosions require removal of the corneal skin and scraping the underlying basement membrane. PRK or PTK can also be used therapeutically to treat recurrent erosions.
Floaters are typically strands of collagen fibers that exist in the vitreous or gel portion of the eye that we see as they move across the visual axis. It’s similar to seeing dust particles floating in a dark movie theater. They look like pieces of a “wrinkled string” or “cobweb” that seem to float in front of a person’s eyes. In most cases, they are harmless and only bothersome. When there is a sudden increase in floaters, flashes of light or a loss of vision, an immediate visit to an eye doctor is required to check for a retinal detachment. Usually there is no treatment performed for floaters because of the risks with surgery. However, very bothersome episodes of floaters can be removed with a surgery called a vitrectomy or with a laser in vitreolysis.
Floaters.pdf

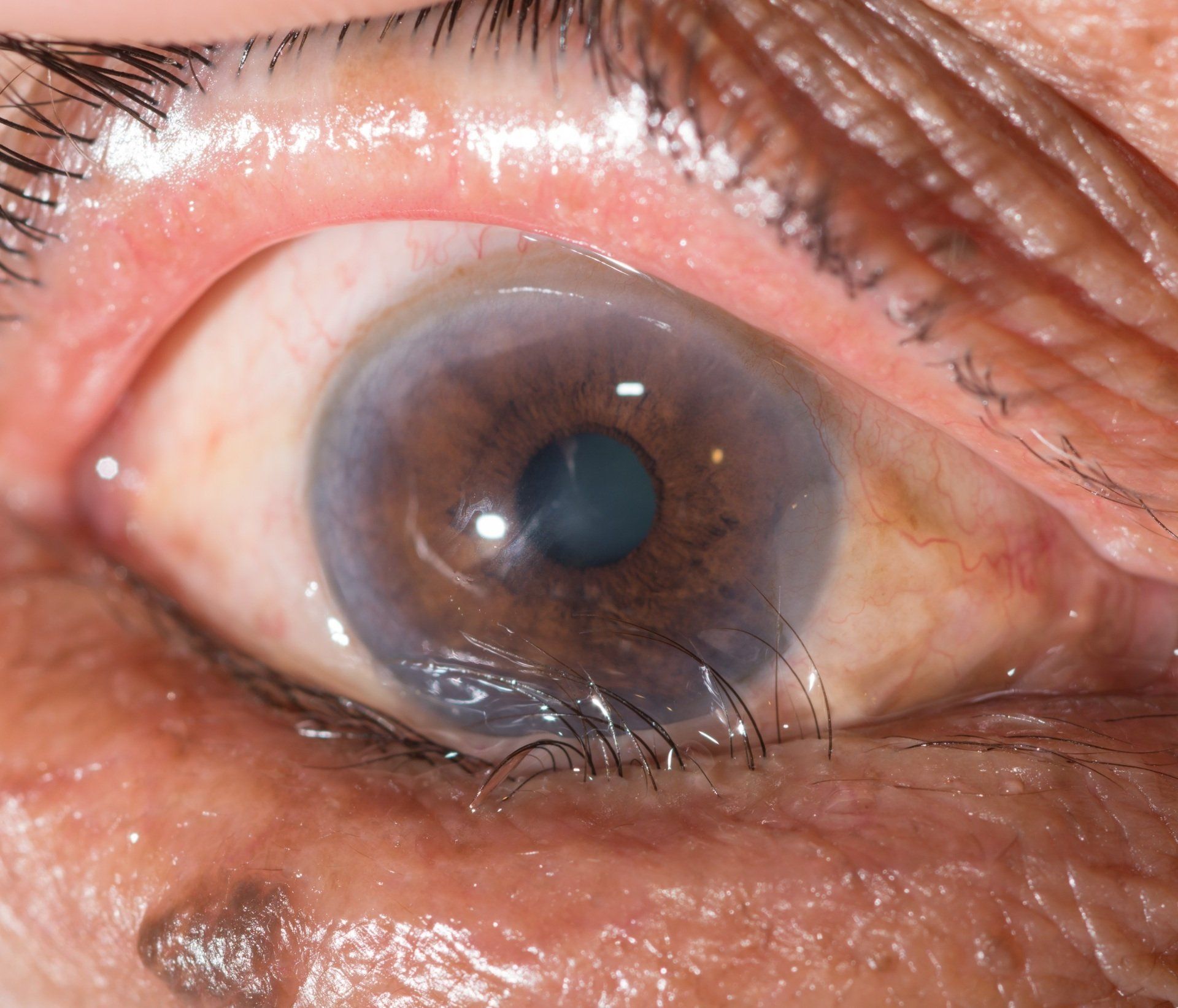
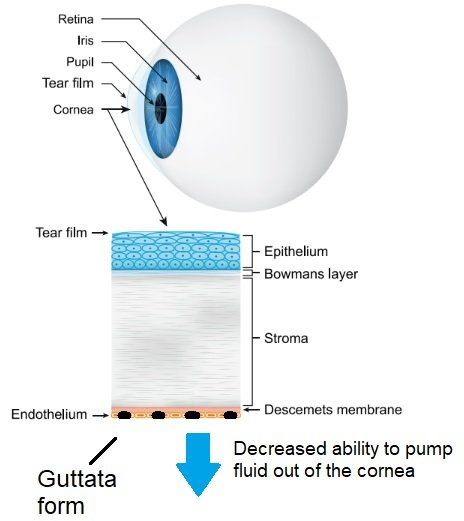
Fuch's Dystrophy
Fuch's Dystrophy is a corneal condition where the endothelial cells on the back of the cornea lose the ability to pump fluid out of the cornea. As the endothelial cells deteriorate they form guttata. When this happens fluid in the cornea builds up causing the cornea to swell and thicken (edema). It results in blurred vision, fluctuating vision, significant discomfort, foreign body sensation and light sensitivity. The condition typically starts in middle-age. It is diagnosed with high magnification on a biomicroscope, pachymetry (measuring corneal thickness) and specular microscopy. Mild symptoms can be treated with hypertonic solutions like Muro 128 to draw fluid out of the cornea. Significant cases require replacement of the corneal endothelial cells with an endothelial keratoplasty procedure (DSAEK and DMEK).
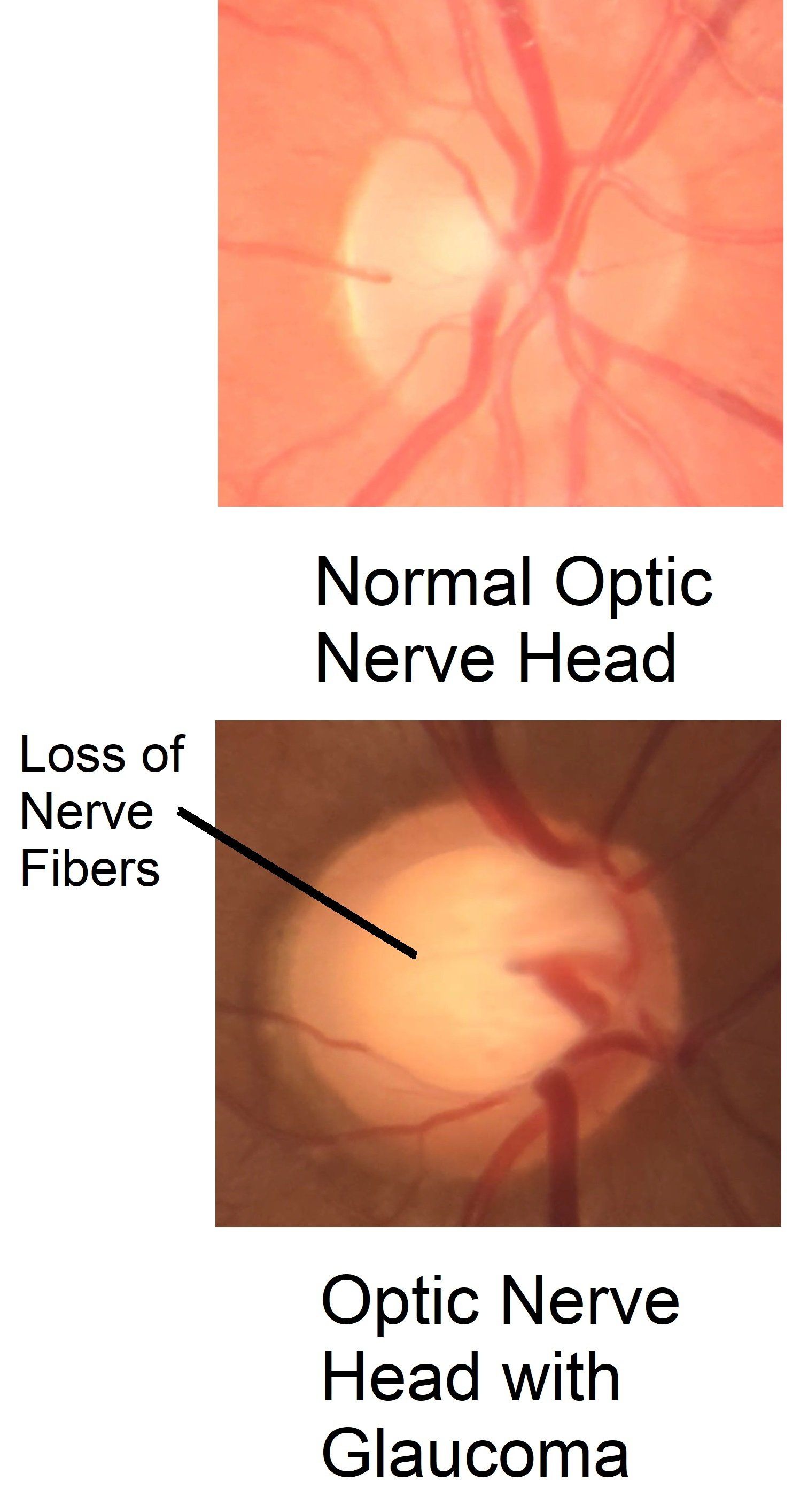
Glaucoma.pdf
Hemangioma
A hemangioma or a "strawberry nevus" is an abnormal overgrowth of small blood vessels on the surface of the skin. They typically grow and appear in the first six months of life. In time they usually disappear on their own. They are found in many different areas in the body. In the eye they are seen on the eyelid, conjunctiva and the eye socket. If they cause the eyelid to cover the eye, they can cause amblyopia in the affected eye. When in the eye socket, they can put pressure on structures in the eye leading to high intraocular pressure and/or optic atrophy. Treatment options include corticosteroids, laser therapy, surgery and beta-blockers.

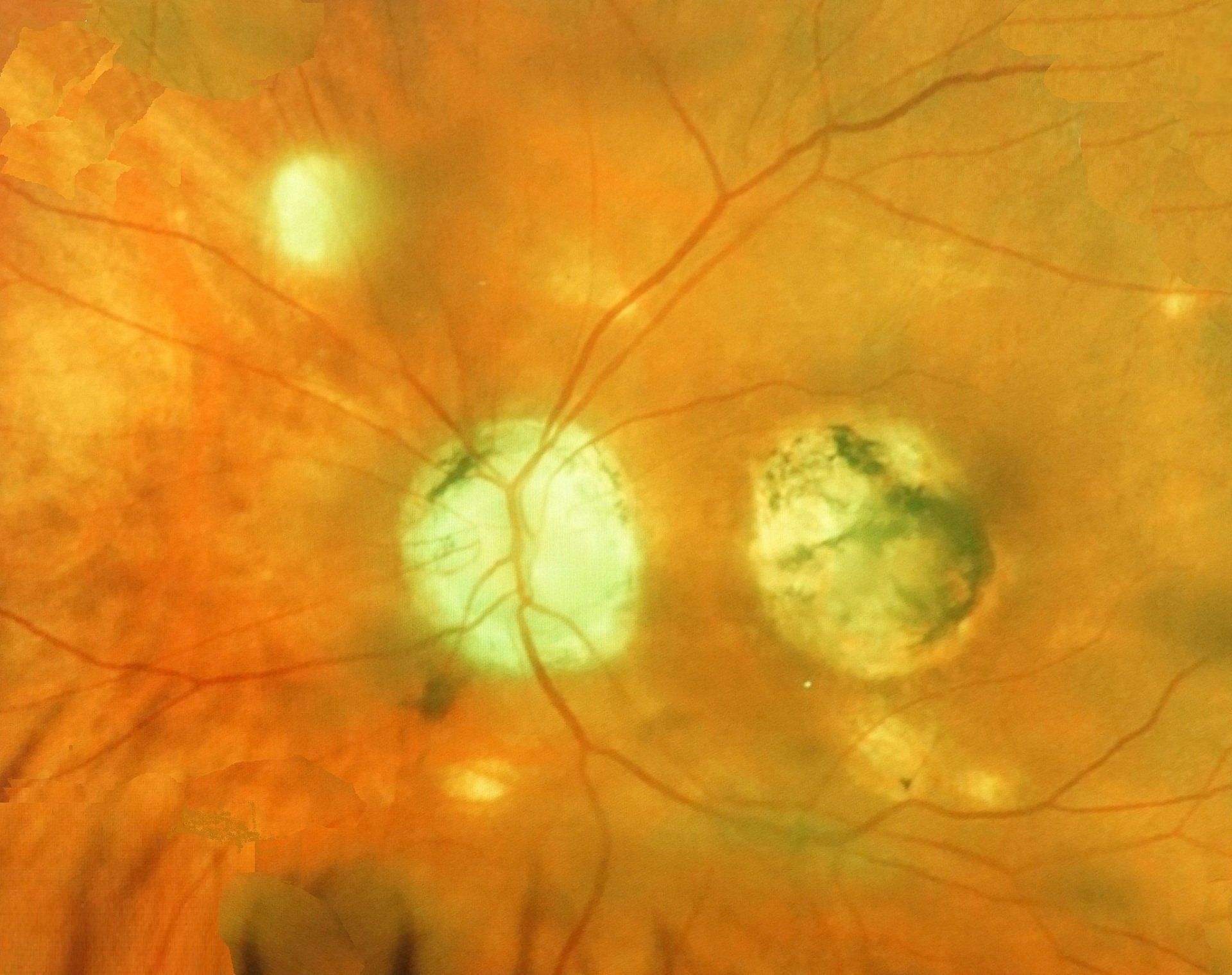
Histoplasmosis
Histoplasmosis is a fungal infection caused by breathing in spores from bird or bat droppings. It is most commonly found in the Ohio & Mississippi River Valleys. The infection starts in the lungs, but can spread to the retina. In the retina the fungus can cause inflammation and scarring. When peripheral aspects of the eye are affected, there is not too much risk of vision loss. However, if they affect the central retina there can be significant vision loss. It is usually found with a dilated fundus exam. In the eye histoplasmosis is treated with anti-VEGF injections and lasers.
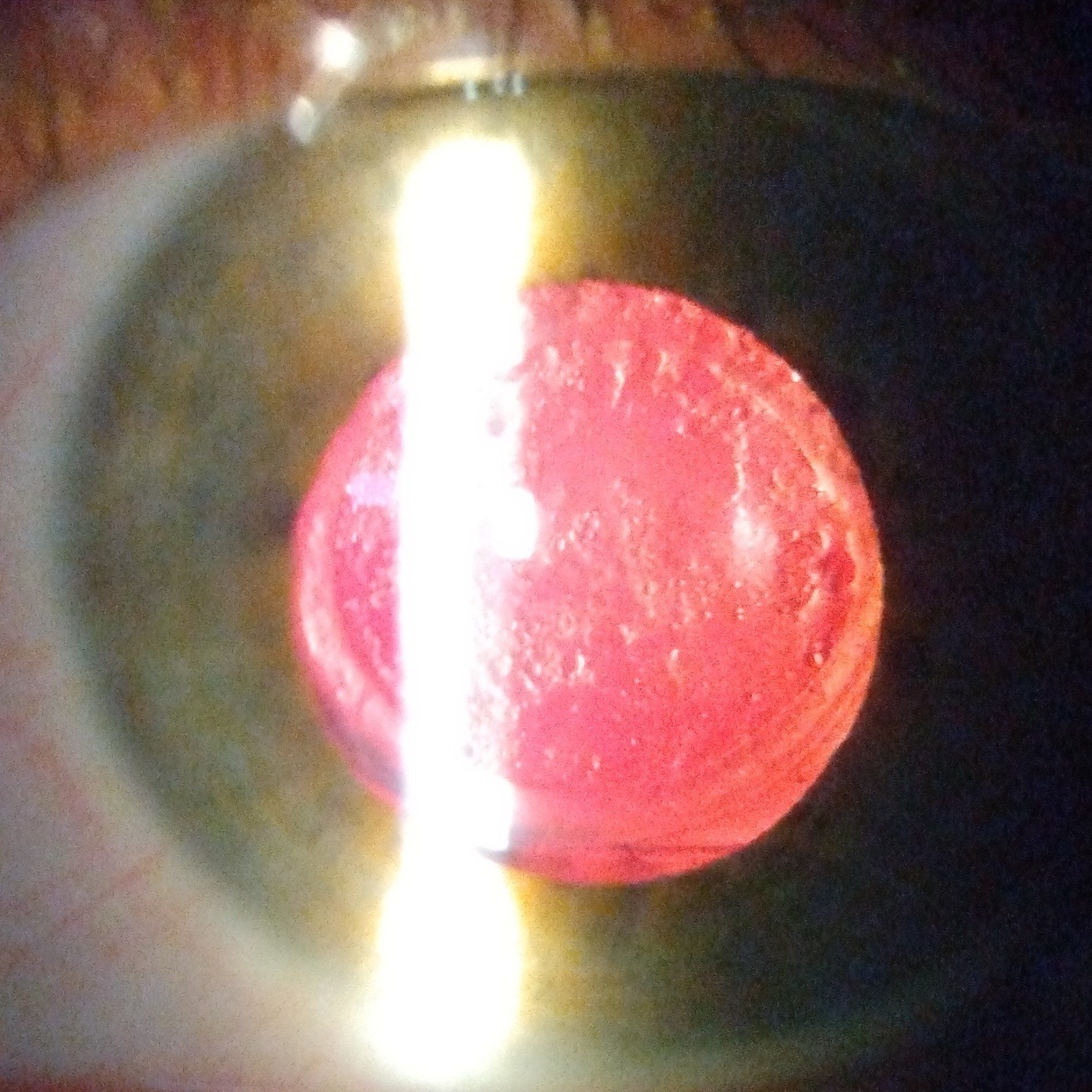
Hyphema
A hyphema occurs when blood collects in the anterior chamber of the eye. Blunt trauma is the most common cause. They can also occur spontaneously with bleeding disorders. They can be prevented with wearing proper eye protection. Often the blood will resolve on its own, however, there is a risk of elevated intraocular pressure and should be evaluated by an eye doctor. If intraocular pressure does increase, the blood may need to be removed or drops might be used to lower the pressure.


Keratitis
Keratitis is inflammation of the cornea. Signs and symptoms include redness, light sensitivity, pain, watering, foreign body sensation and decreased vision. It has both non-infectious and infectious causes. Non-infectious causes may be related to trauma, exposure, surgery or autoimmune disorders. Infectious causes are typically viral or bacterial (rarely fungal or parasitic). Evaluation of keratitis is obtained by taking a good medical history, testing vision and carefully examining the eye with a biomicroscope. Treatment for non-infectious keratitis uses topical NSAID and steroid medications. Infectious keratitis is treated with the appropriate antiviral or antibiotic. Steroids might be used with infectious keratitis once it has been determined that they wouldn’t make the infection worse.
Lattice Degeneration
In lattice degeneration there is a thinning of the peripheral retina. It is more common in patients with myopia. This is likely related to the stretching of the peripheral retina that occurs with axial elongation in myopia. In most cases patients aren't even aware that they have it and it is seen during a dilated fundus exam. The biggest concern with lattice degeneration is that they may lead to breaks, holes, tears and possible retinal detachments. For this reason it is a good idea to get a dilated fundus exam every year, if you have it.
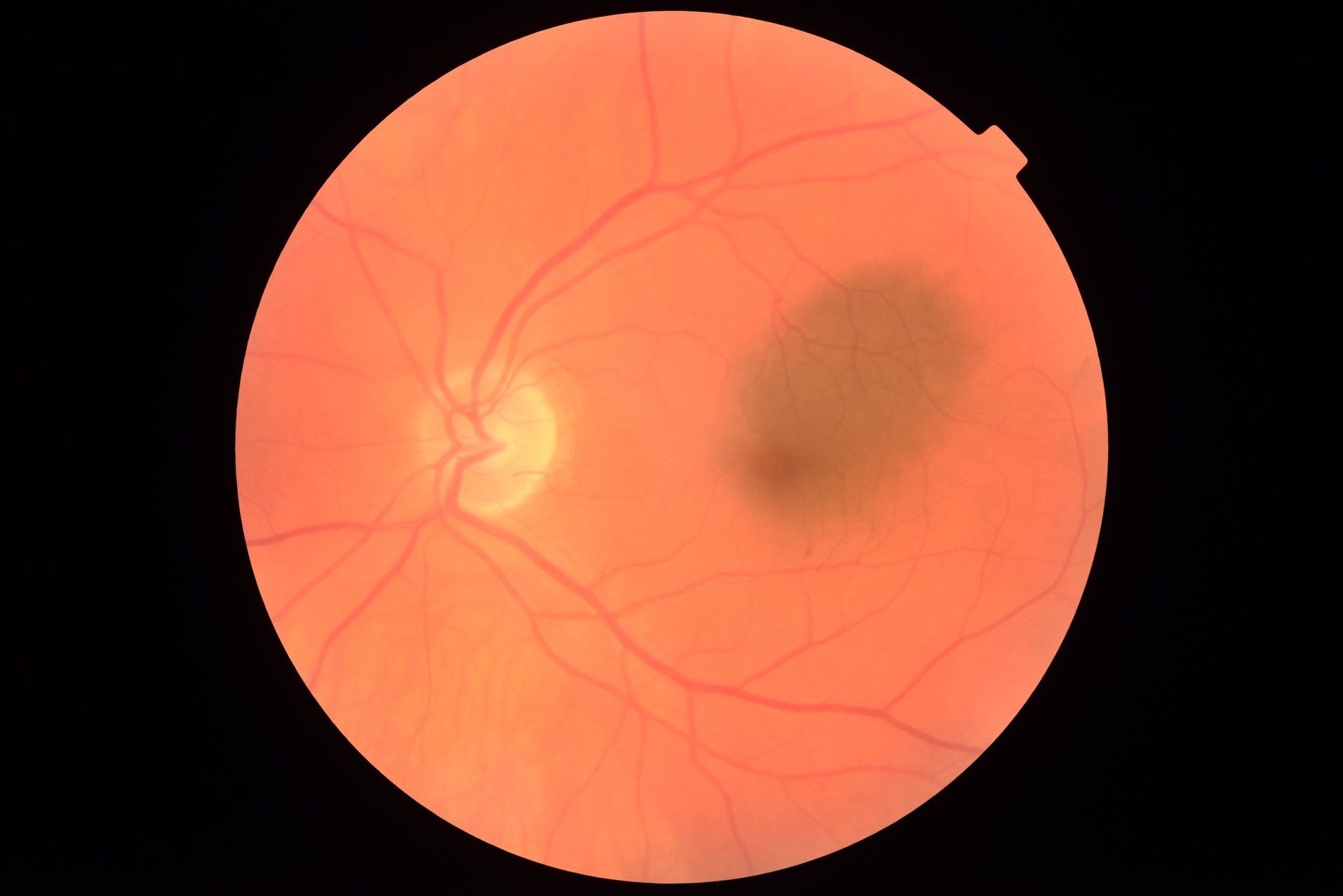
Macular Hole
A macular hole is a hole that forms in the central part of the retina called the macula. They are much more common in the age group of 60 years and older. If vision is good in one eye, you may not notice any symptoms of a macular hole in early stages. However, as the condition persists lines may become distorted and the center of what you’re looking at is not seen. A frequent cause of these is the vitreous pulling on the macula. They are more common with myopia, ocular injury, macular pucker, uncontrolled diabetes and posterior vitreous detachments. A vitrectomy is done to treat macular holes to stop the vitreous from pulling on the macula. Early treatment has good visual outcomes. When a macular hole has been present for more than a year, visual outcomes are much poorer.
Myokymia
Myokymia is a fluttering or twitching of the eyelids. It is caused by a muscle spasm in the muscle that surrounds the eye. They are related to poor sleep, stress and bad nutrition. In most cases, they are only a slight annoyance and resolve on their own. In severe cases that develop into a blepharospasm Botox injections are commonly done.
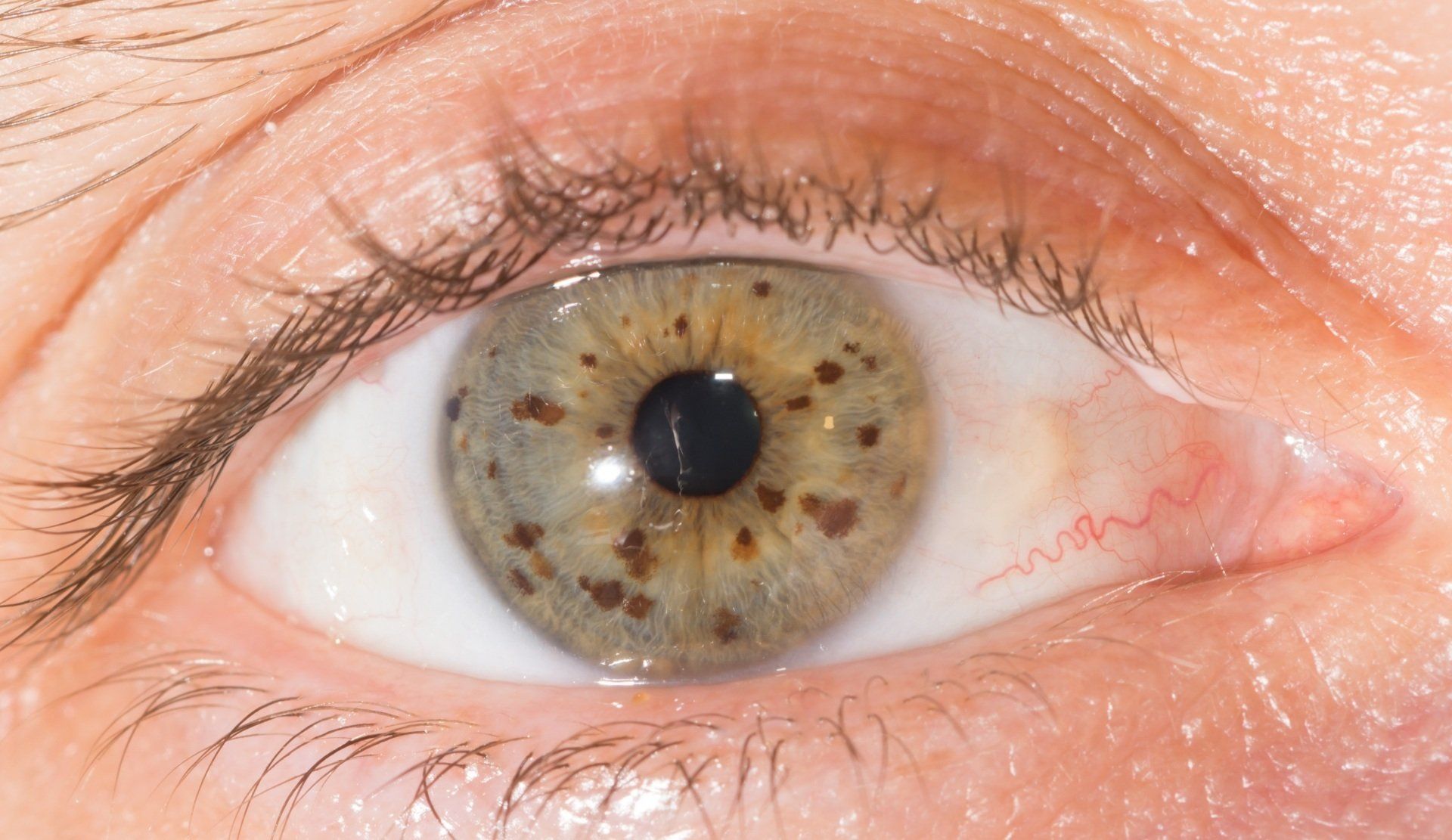
Nevi
Nevi or "freckles" are very common on the eye. They are seen on the conjunctiva, iris and choroid in the retina. In the vast majority of cases nevi in the eye are benign and can be safely monitored. However, like a "freckle" on the skin they can turn into melanoma in the eye. A nevus that is large, changes in size, shape or color should be evaluated thoroughly.
Nystagmus
Nystagmus is a rapid and involuntary shaking or moving back and forth of the eyes. Individuals with it typically have decreased vision, dizziness and disorientation. Sometimes individuals hold their head in a certain position to reduce the nystagmus. Early in life it is caused by poor development of the visual system. Later in life nystagmus is associated with trauma, certain medications, inner ear problems, strokes or other conditions affecting the brain. Treatment consists of getting the proper visual correction and treating the underlying cause, if possible.
Ocular Migraines
Ocular migraines or migraine auras are visual disturbances that affect both eyes. These types of migraines are short-lived, can occur in isolation, precede or happen with a migraine. Most don’t last more than 30 minutes. In some cases, they affect speech, motor functions and other senses. When they happen for the first-time people find them very disturbing and concerning.
Triggers to ocular migraines are similar to triggers for migraines. The exact cause of ocular migraines is not known. They could possibly be related to blood vessel spasms in the retina and the visual pathway.
An eye exam is a great starting point to evaluate the symptoms of an ocular migraine and to rule out other possibilities like a retinal detachment or amaurosis fugax. Further evaluation should also be done by a neurologist. Potential treatments include tricyclic antidepressants, anti-seizure medications, NSAIDS (ibuprofen or naproxen) and triptans.

Ocular Toxoplasmosis
Ocular Toxoplasmosis is caused by a parasite called Toxoplasma gondii. The parasite can be spread during pregnancy or acquired after birth. When in the retina it will multiply and break open host cells leading to infections in surrounding cells. Oftentimes the parasite is contained by the host's immune system. Patients with Ocular Histoplasmosis can lead to increased intraocular pressure, light sensitivity and pain. When in the macular region of the retina central vision loss can be significant. Testing for Ocular Histoplasmosis includes a dilated fundus exam and blood tests for antibodies to the parasite. Patients will experience decreased vision, inflammation, pain, redness, sensitivity to light, blurred vision, and increased intraocular pressure. Treatment consists of antiparasitic and corticosteroids to eliminate the parasite and control the resulting inflammation. Without treatment significant vision loss can occur.
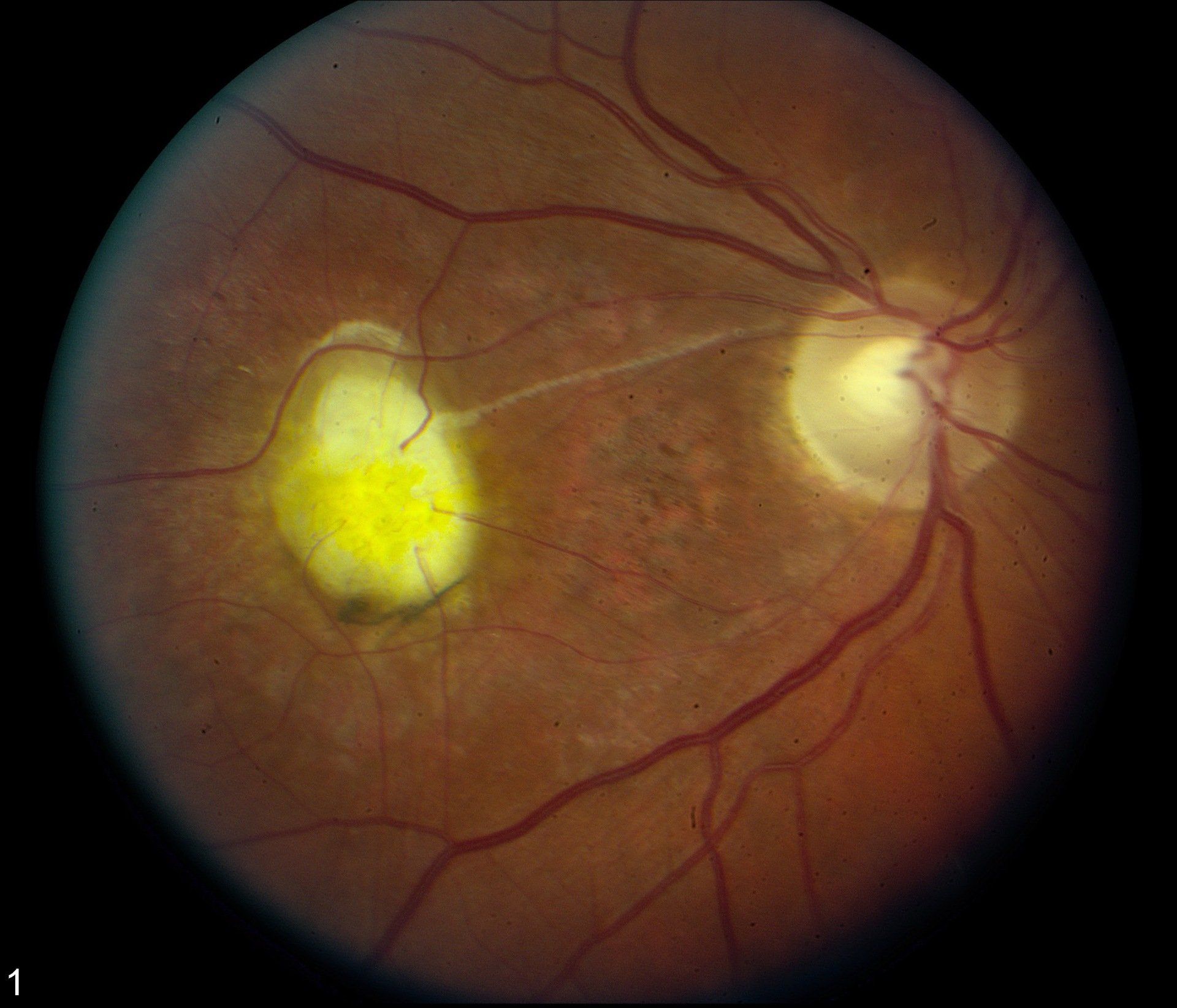
Optic Nerve Head Drusen
Drusen on the optic nerve head (ONH) are abnormal yellowish growths made up of a combination of lipids and proteins that calcify as we age. They may give an appearance of ONH swelling or elevation. Because of this it should be distinguished between papilledema. Most patients with ONH drusen are unaware that they have them. There can be mild visual field loss and headaches as a result. Evaluation includes a dilated fundus exam, fundus photography, B-scan ultrasonography and visual field testing. There is no effective treatment for ONH drusen.

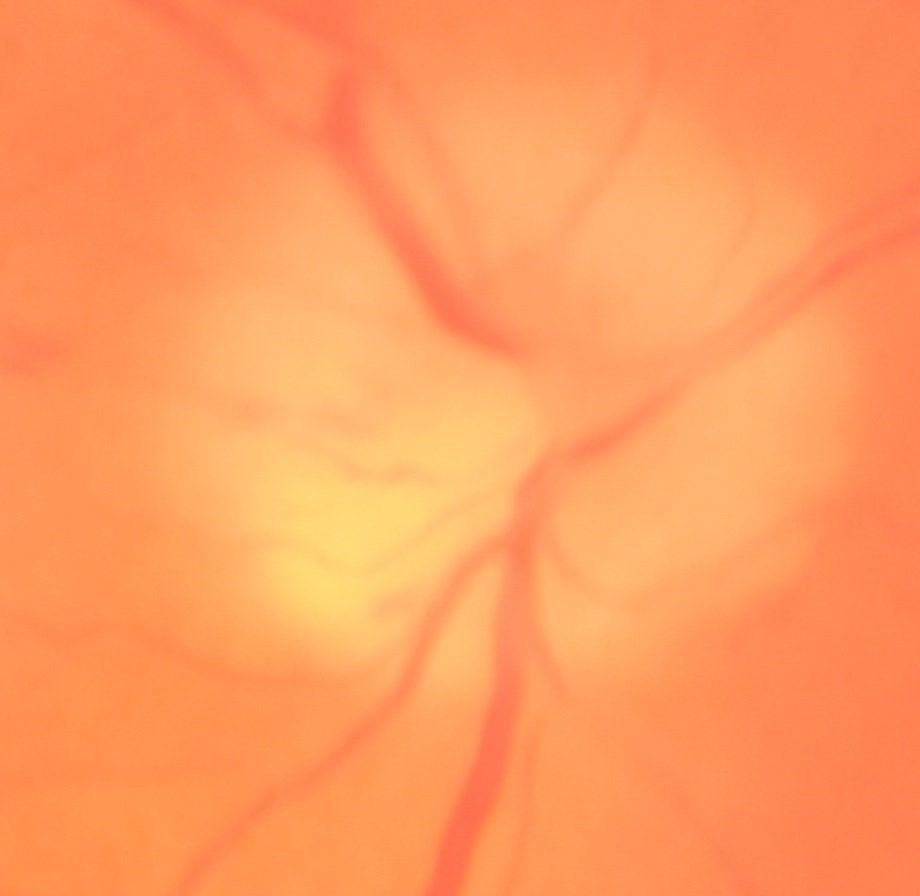
Optic Neuritis
Optic neuritis is inflammation of the optic nerve. The optic nerve carries nerve signals from the eye along the visual pathway into the brain. Symptoms of it include decreased vision, loss of peripheral vision, pain with ocular movement and diminished color perception. Optic neuritis is caused by multiple sclerosis, other auto-immune diseases, viral and bacterial infections. Evaluating optic neuritis includes a dilated fundus exam, visual field testing, MRI scans and laboratory testing. Treatment involves treating the underlying cause that may include intravenous steroids, antibiotics and antivirals.
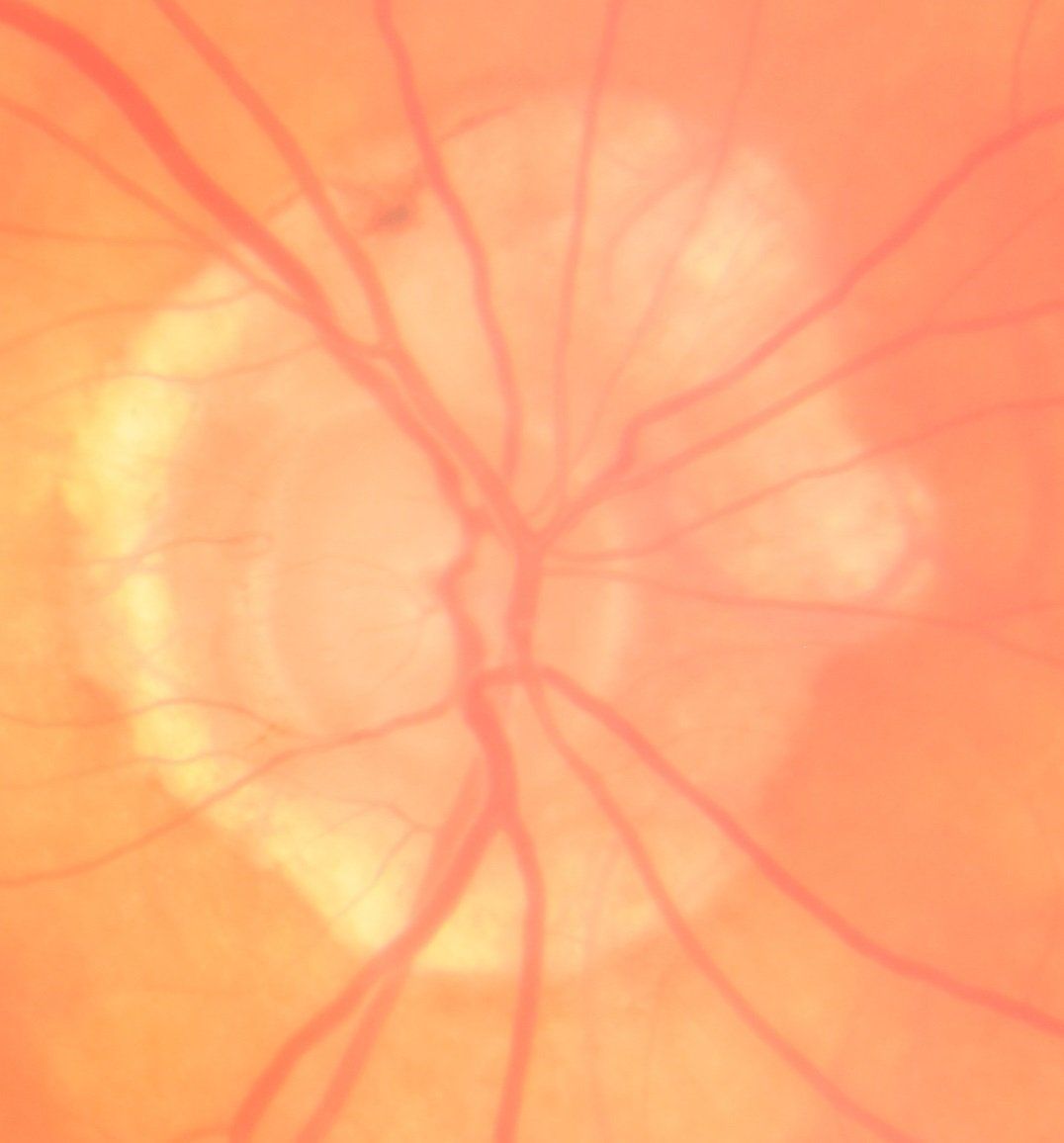
Papilledema is a swelling of the optic nerve head caused by elevated intracranial hypertension. Symptoms include headaches, nausea, decreased vision, double vision and visual field loss. Your eye doctor will notice elevated and blurred optic nerve head margins. Blood vessels coming from the optic nerve are also engorged. The most common causes of papilledema include brain tumors, poor absorption of the cerebral spinal fluid or medications. Treatment consists of managing a tumor if present, diuretics, losing weight and removal of any causative medications.
Papilledema.pdf

Papilloma
Papilloma are common benign skin growths that form because of degeneration of the skin around the eye. The incidence of papilloma increases with age. In some cases, they can cause mild irritation and redness. If patients are not bothered by them, they can simply be monitored for changes in size, shape or color. However, if the patient is bothered by the growth, it can be removed surgically. If a type of skin cancer is suspected, samples should be sent for evaluation. Growths on the lid margin should be referred to an oculoplastic surgeon to avoid causing problems with the blink and ocular surface disease.

Pathological Myopia
Pathological myopia or degenerative myopia is a state where there is a very large amount of myopia (greater than 6.0 diopters) in an eyeglass prescription. It is a result of elongation or enlargement of the eye. This deformation of the eye causes stress to the retina and its associated structures. The retina is pulled away from the optic nerve head and forms a myopic ring. Lattice degeneration and its associated risk of a detached retina are significantly more common in pathological myopia. Posterior staphylomas can develop and thinning of retinal support cells also occurs. These changes lead to highly myopic eyeglass prescriptions, decreases in best corrected vision and increased risks of retinal problems. An eye doctor will need to do a dilated fundus exam or wide-field fundus photography to evaluate an eye with pathological myopia. A direct cause of myopia has not been found. However, it has a genetic component and increases in those that spend more time indoors. Treatment of pathological myopia includes yearly dilated eye exams to watch for potential complications. Diluted atropine drops can also be used to slow the progression of myopia in children.
Pigment Dispersion Syndrome
Pigment dispersion syndrome (PDS) occurs when pigment in your iris rubs up against the lens zonules and then floats around the anterior chamber of the eye. Oftentimes you can get iris transillumination of the iris where the red glow of the retina shows through the iris. Pigment is seen on the back of the corneal endothelium and in the chamber angle where fluid drains out of the eye. When the pigment "clogs" the drainage out of the eye, it can lead to increases in intraocular pressure and potentially glaucoma. Patients with PDS should have a yearly eye exam with measurement of intraocular pressure and evaluation for glaucoma.
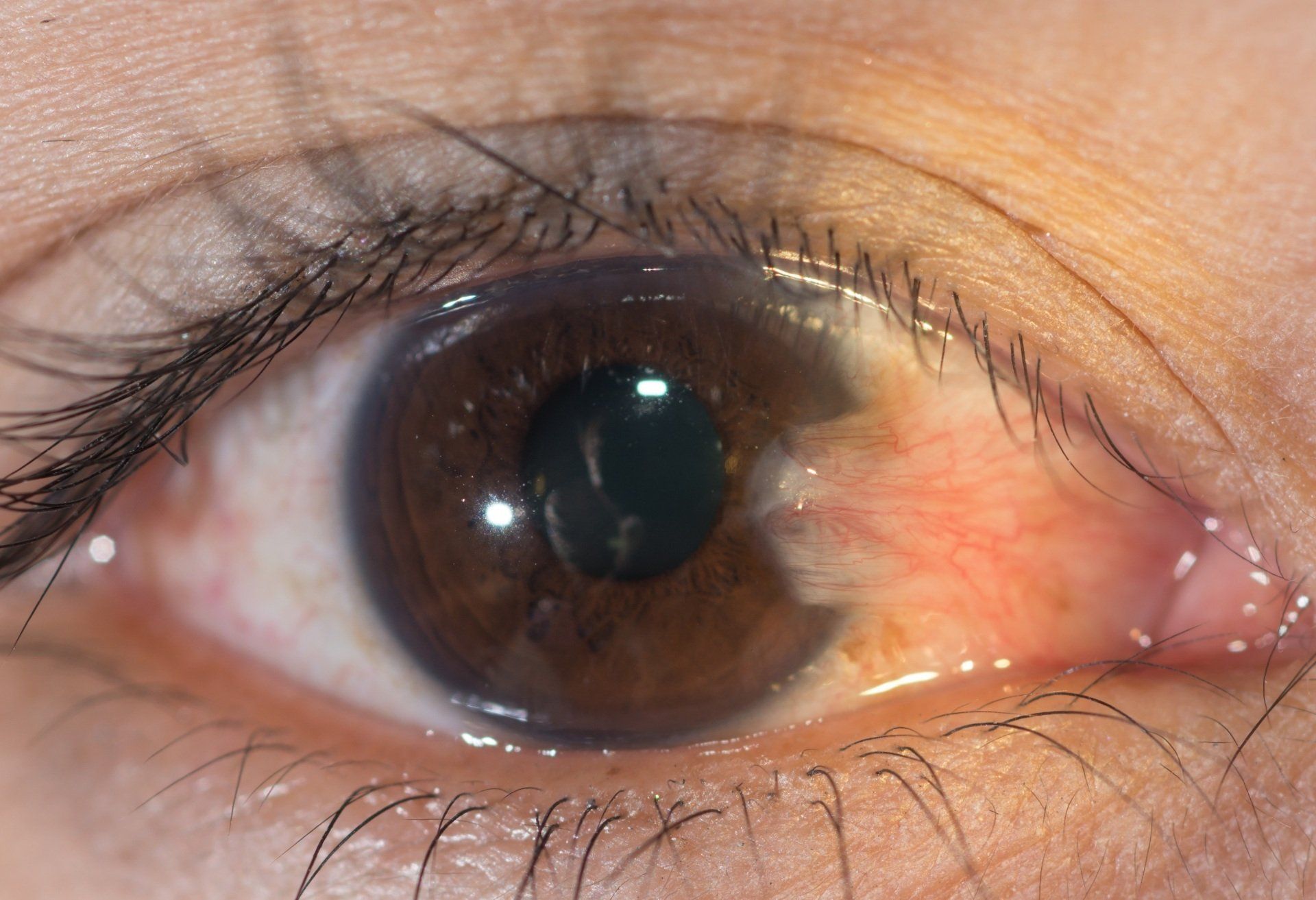
Pinguecula
A pinguecula is a small, elevated growth on the conjunctiva with a white to yellow color. They can grow on the nasal or temporal side of the eye. In most cases there are no symptoms. In those that do have symptoms they include redness, foreign body sensation, scratchiness and irritation. Pinguecula are the result of exposure to UV light from the son. As they advance a pinguecula can turn into a pterygium and start growing over the cornea. There is usually no recommended treatment for pinguecula unless the patient is having symptoms. In that case ocular lubrication, UV protection, anti-inflammatory drops and surgical removal. If they are removed with surgery, recurrence rates are high.
Posterior Capsular Opacification
A posterior capsular opacification (PCO) or secondary cataract is a common problem after cataract surgery. Symptoms of a PCO include decreased vision, glare, haloes and double vision. They are caused by remnant lens cell migration and proliferation inside of the lens capsule. The best way to evaluate them is with a dilated eye exam and evaluation with a biomicroscope by your eye doctor. Treatment is done with a YAG laser to open holes in the lens capsule.
Posterior Vitreous Detachment
A posterior vitreous detachment (PVD) happens when the gel or vitreous in the eye condenses and pulls away or separates from the retina. They are very common as we age. Symptoms include seeing floaters and flashes. To evaluate a PVD you eye doctor will dilate your eyes and look thoroughly to make sure the vitreous is pulling on any part of the retina. In rare cases a PVD is associated with macular holes and retinal holes. Almost all PVD's are monitored and only treated with retinal complications.
Pseudoexfoliation Syndrome
Pseudoexfoliation syndrome is caused by a slow accumulation of a fibrillar material from the crystalline lens that collects on the structures in the anterior chamber of the eye (the lens itself, zonules, iris, chamber angle and corneal endothelium). It is more common with age (60 years and older) and with Mediterranean and Scandinavian ancestry. The biggest concern with pseudoexfoliation is that it can "clog" the drainage of fluid in the anterior chamber angle. This can lead to increases in intraocular pressure and potentially glaucoma. Patients with Pseudoexfoliation should have a yearly eye exam with measurement of intraocular pressure and evaluation for glaucoma.
A pterygium or “surfer’s eye” is an overgrowth of tissue that grows from the conjunctiva onto the cornea. It is the result of tissue that degenerates from exposure to ultraviolet light and the windy environments. Most often they have a triangular shape and are very vascularized. They are mostly cosmetic and only need to be monitored for growth or any impact on vision. When significant, they induce mild to large amounts of astigmatism. If they grow over the visual axis, there can be loss of best corrected visual acuity. Treatment consists of UV protection, ocular lubrication and surgical removal. Even with removal re-growth can occur.
Ptosis
Ptosis is a dropping of the upper eyelid. It is caused by damaged or weakened muscles that elevate the upper lid. It can also be caused by damage to the nerves that innervate those muscles. Ptosis has varying degrees, but when it covers the pupil or significantly blocks the upper visual field surgical intervention is needed. It affects both adults and children.
A retinal detachment is a very serious condition where the sensory layer inside of the eye called the retina tears, pulls or separates from the eye. If it is not treated promptly, permanent vision loss or blindness can occur. Symptoms of a retinal detachment include flashes of light, loss of vision and numerous new floaters. Causes of a retinal detachment include ocular trauma or surgery, high amounts of myopia, vitreous traction (the jelly-like portion of the eye pulling on the retina) and conditions that cause abnormal bleeding in the eye. To assess for a retinal detachment the eyes need to be dilated and then a thorough look at all parts of the retina needs to be done. Treatment involves injecting a gas bubble in the eye forcing the attached retina in place or suturing a sponge to the white portion of the eye that prevents further traction from the vitreous. Lasers or freezing are sometimes used to scar areas of the retina to prevent a detachment or limit further detachment.
Retinal Detachment.pdf

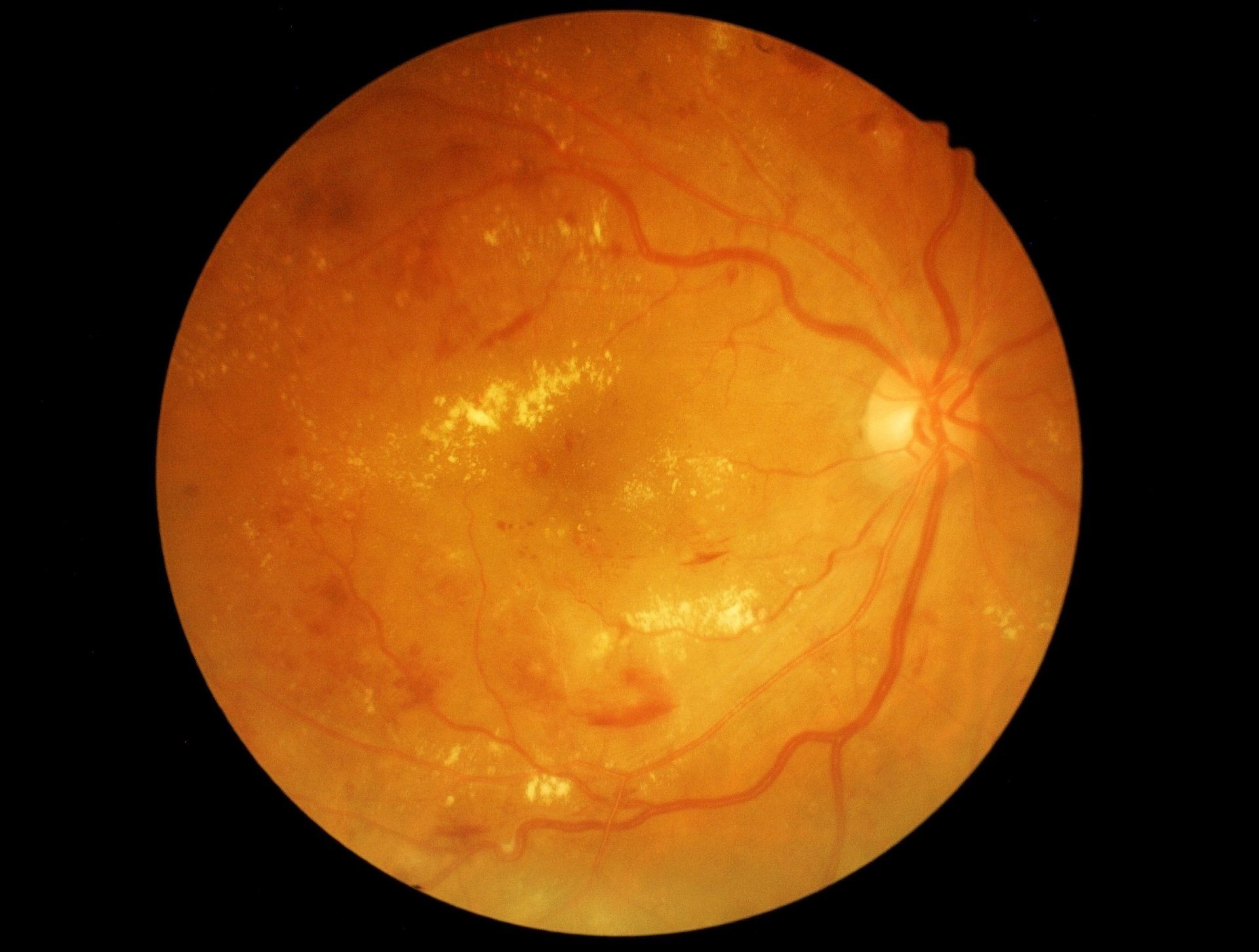
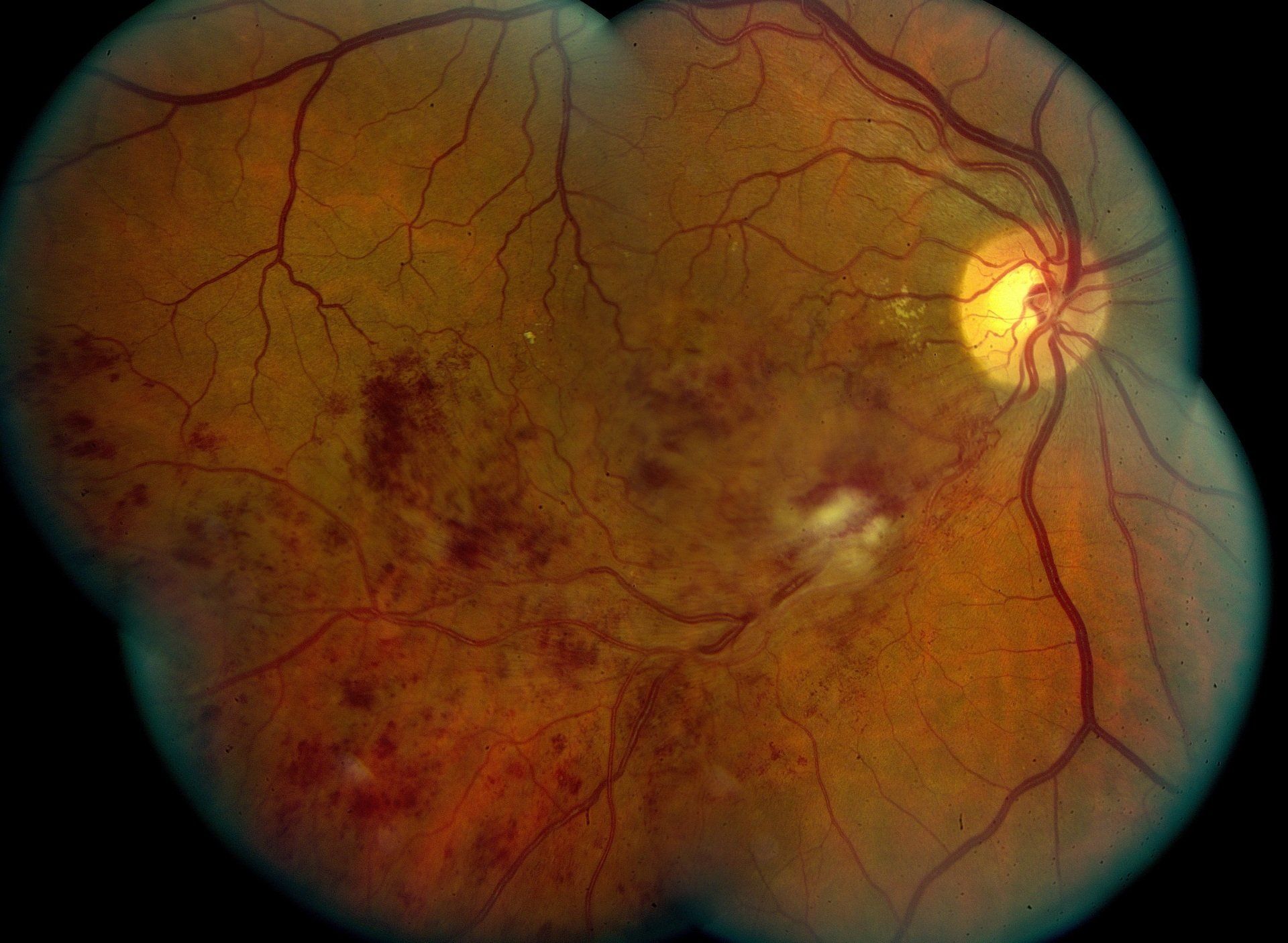
Retinal Vein Occlusion
A retinal vein occlusion occurs when there is a blockage of a vein carrying blood away from the retina. The blockage leads to bleeding and swelling in the retina. Patients will notice a significant decrease in the vision of one eye. They are often the result of significant hypertension, uncontrolled diabetes, high cholesterol and bleeding disorders. Your eye doctor will see hemorrhages, swelling and potentially macular edema. A fluorescein angiography and OCT are done to evaluate the extent of the retinal vein occlusion. Treatment consists of managing underlying causes like controlling blood sugar and reducing blood pressure. Management by a retinal specialist often includes intravitreal injections of anti-VEGF and steroids. Other treatments may include lasers to treat neo-vascularization.
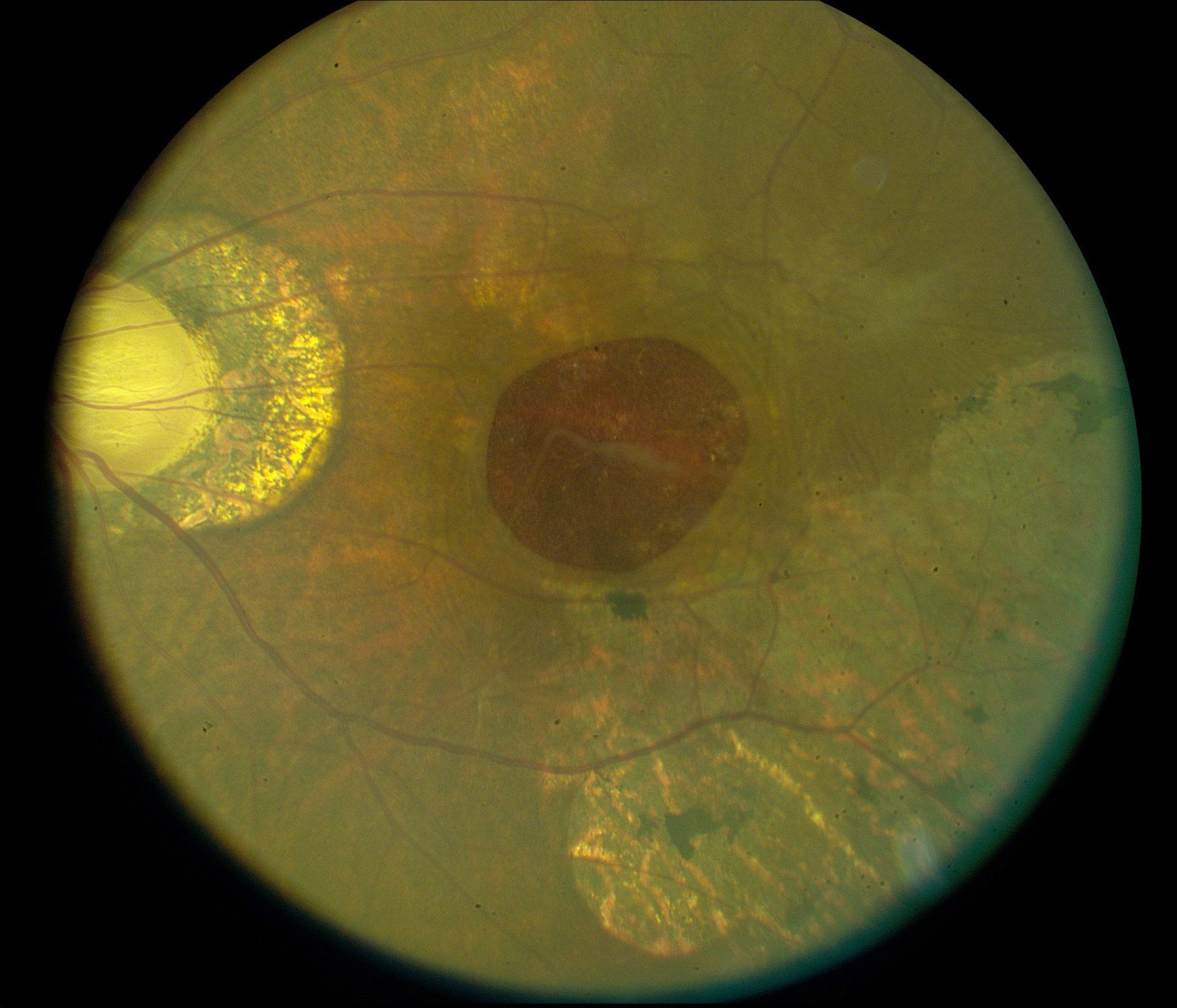
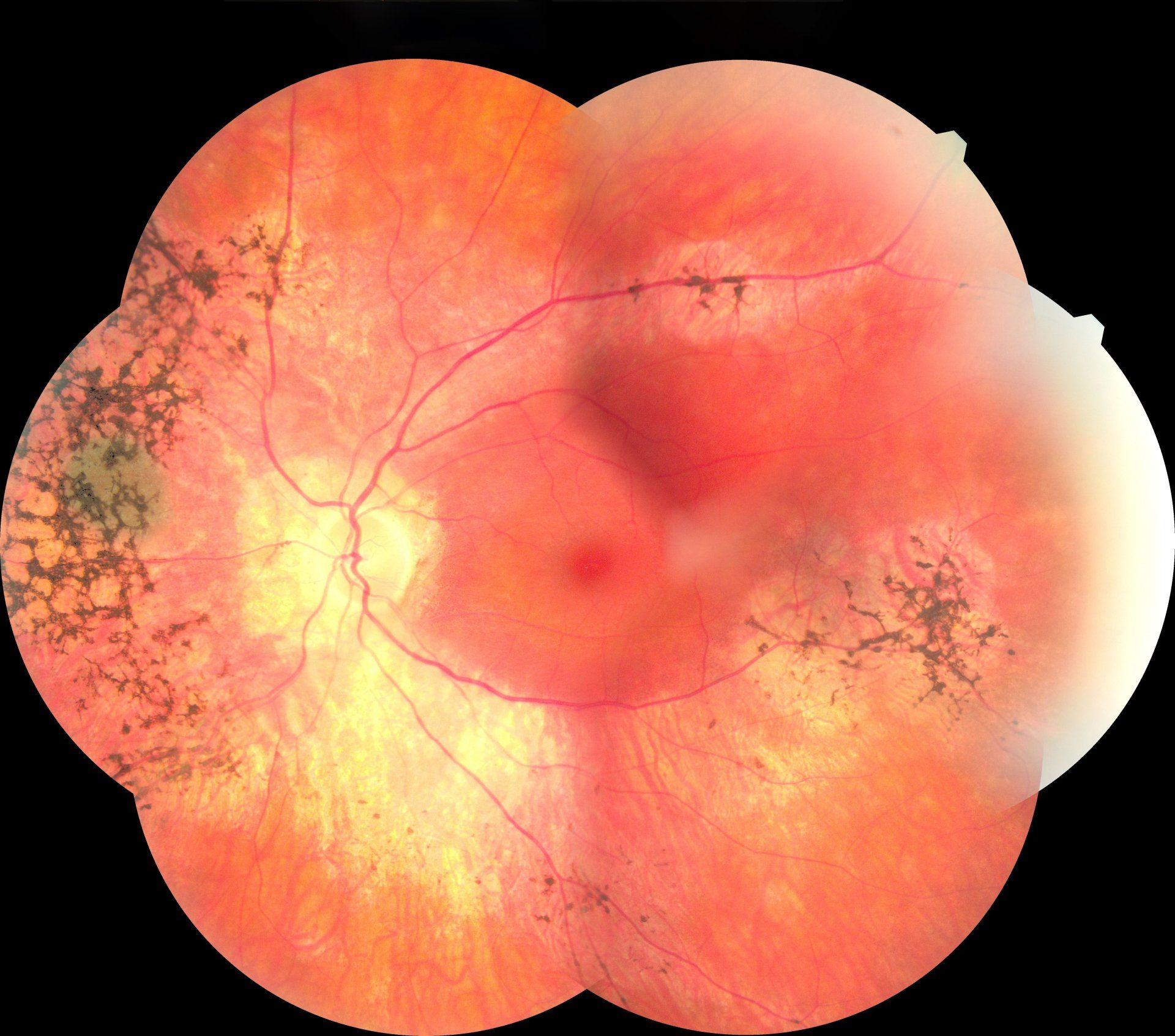
Retinitis Pigmentosa
Retinitis Pigmentosa (RP)is a genetic condition of the eye with varying inheritance patterns that starts as a child and eventually progresses to blindness. Early on in patients with RP, night vision is difficult. They have a difficult time moving around in low light levels. There is also a loss of peripheral vision and then eventually central vision. It is caused by a gradual deterioration of the photoreceptors and their supportive pigment cells in the retina. Evaluating RP includes a dilated fundus exam, visual field testing, fundus photography, potentially a fluorescein angiography and genetic testing. Treatment is limited to providing correct spectacle correction and low vision services.
Scleritis
Scleritis is inflammation of the sclera or white part of the eye. It is typically very painful and will present with an inflamed red eye. The eyes water, vision can be diminished and light sensitivity are other common symptoms. Scleritis is caused by an overactive immune system and is related to conditions like Rheumatoid Arthritis or Lupus. Treatment often includes ibuprofen (NSAIDs), corticosteroids (topical and pills) and antibiotic/antiviral medications, if appropriate. Early treatment is important to prevent progression. Moderate and advanced cases are best managed by a specialist.
Strabismus or a tropia is a misalignment of the eyes, meaning that they don’t look at an object together. An eye can turn in, out, up or down. A long standing strabismus may not have any symptoms because the brain shuts off or “suppresses'' the image from the eye that turns away. A new onset results in double vision and disorientation. Strabismus occurs because of poor coordination between the extraocular muscles or the nerves that innervate them. Testing done by your eye doctor includes a cover test to assess ocular alignment, determination of refractive state and an assessment of ocular health. Treatment involves the use of prism in glasses, vision therapy, surgery and correction of refractive error.
Strabismus.pdf

A stye is an infection of an oil gland on the eyelid margin. They are also called an internal hordeolum. They usually present as a painful, red bump on the eyelid. They are frequently associated with blepharitis and rosacea. Staphylococcal bacteria are the most common organism to cause the infection. In many cases they resolve on their own. Treatment consists of a warm compress to loosen inflammatory material and to open up pores 4-5 times a day. Massaging the stye may also be beneficial to help express the material inside it. Lid scrubs with baby shampoo and water are important to clear the eyelid margin of bacteria. This will reduce the recurrence. Without resolution oral antibiotics should may be given and in some cases they may require drainage.
Stye.pdf

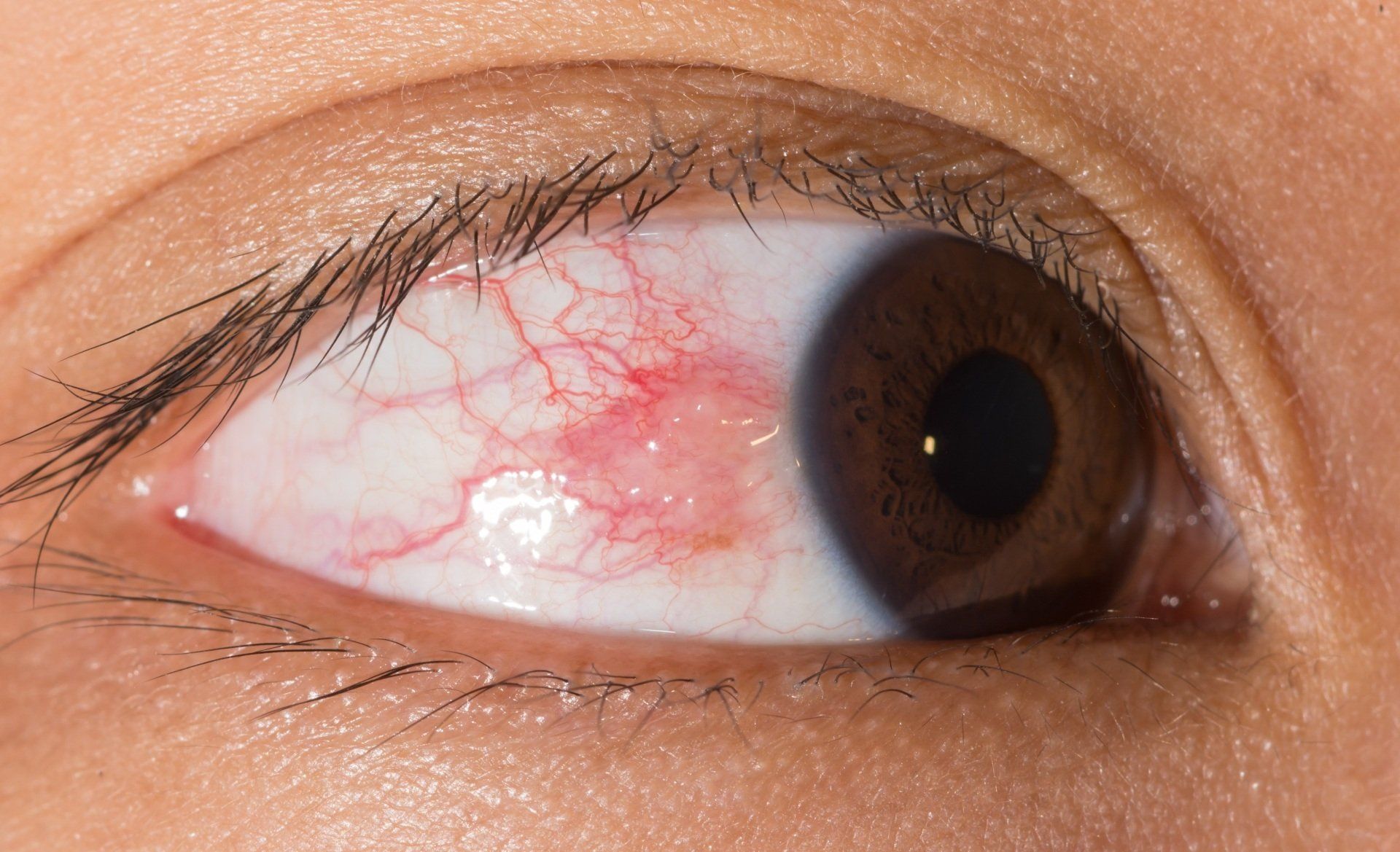
Subconjunctival Hemorrhage
A subconjunctival hemorrhage occurs when a blood vessel in the conjunctiva (the mucous membrane of the eye). The blood essentially gets trapped in the conjunctiva and doesn't resolve quickly. It takes time for the blood to disappear. They happen with straining, vomiting, trauma and rubbing the eye. Risk factors for a subconjunctival hemorrhage include diabetes, hypertension, taking blood thinners and having blood clotting conditions. If they reoccur it is appropriate to perform blood testing of platelets and clotting factors. There is no real treatment other than monitoring them for recurrence.

Thyroid Eye Disease
Thyroid eye disease or Grave's Disease is considered to be an auto-immune condition where our own immune system attacks structures in the eyes. Symptoms include dry eyes, redness, decreased vision, double vision and bulging eyes (as seen in the accompanying image). Antibodies end up attacking the thyroid and the soft tissue behind the eyes. From this the soft tissue and muscles behind the eyes become engorged and force the eyes to bulge out of the eye socket. Evaluation includes testing thyroid blood levels and antibodies. Other tests include measuring iodine uptake, ultrasound of the thyroid, exophthalmometry, and imaging of the eyes and thyroid. Common treatments include radioactive iodine and thyroid removal.

Xanthelasma
Xanthelasma is a yellowish growth that occurs in the corner of your eyelids by the nose. They are caused by a collection of cholesterol deposits under the skin. They are not harmful and mostly cosmetic. They are more common in those that are diabetic, overweight, have a high cholesterol or drink a lot of alcohol. Removal is done with surger, lasers, chemical peels and cryotherapy. Because of the delicate lid structures around the eye it is best for them to be removed by an oculoplastic surgeon.

